With the recent FDA approval of a buprenorphine extended release injection, it seemed like a perfect opportunity to discuss practical issues with this new dosage form and how it could change the way buprenorphine is prescribed and administered to patients requiring long-term buprenorphine for the FDA indication of opioid use disorder. According to the professional package insert, “Sublocade is indicated for the treatment of moderate to severe opioid use disorder in patients who have initiated treatment with a transmucosal buprenorphine-containing product, followed by dose adjustment for a minimum of 7 days. It should be used as part of a complete treatment plan that includes counseling and psychosocial support.”
The applicability and questions in my mind have far broader implications. Here to briefly review those implications is Ms. Caroline Breen, a student pharmacist soon to graduate as a doctor of pharmacy.
Sublocade is the first once-monthly extended release buprenorphine injection that was recently approved by the FDA for moderate to severe opioid use disorder. It is approved for adult patients who have been stable on trans-mucosal buprenorphine (8 to 24 mg equivalent daily) for at least seven days.1

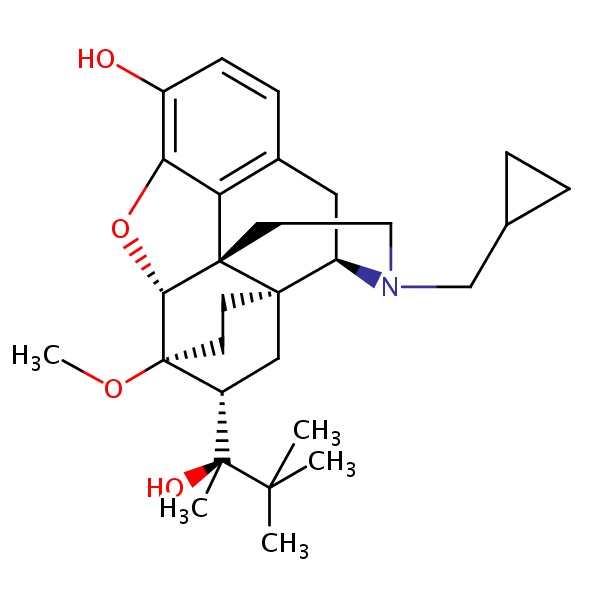
Buprenorphine is a partial agonist at the mu-opioid receptors, and also an antagonist at the kappa receptors. The activity at the mu-opioid receptors is responsible for buprenorphine’s analgesic effect. By blunting the drug-liking or the pleasure effect, it provides its positive benefit in opioid use disorder. Buprenorphine also has utility as a potent analgesic and could be especially beneficial for pain patients requiring long-term opioid therapy. In fact, once it is decided to place a patient on opioids chronically, buprenorphine is the safest most logical first step prior to a full agonist. Unfortunately, that is unlikely to occur in a profit-driven medical system. Moreover, if a patient requires long-term opioid therapy for pain and there is a history of opioid abuse or taking extra doses, a once monthly injection could help foster compliance. Buprenorphine’s partial agonism results in a “ceiling effect” on CO2 accumulation and resultant respiratory depression. All opioids inhibit the carbon dioxide feedback loop that stimulates the brainstem to increase respiratory rate. With most opioids, increasing the dose results in greater inhibition of this feedback loop. Buprenorphine however, reaches a point where increases in dose do not result in more inhibition to the feedback loop. Thus, it is a safer alternative for patients at risk for respiratory depression. Various buprenorphine products are currently approved for either opioid use disorder or pain, but at lower doses in pain. No product is FDA approved for both. 2,3 These products were reviewed in a Pharmacy Times review by Dr. Fudin and colleagues approximately two years ago.
Sublocade delivers a sustained plasma level of buprenorphine with the once monthly injections. Currently, the recommended dosing regimen is 300mg monthly injection for the first two months, followed by the maintenance dose of 100mg monthly. If a patient is not showing enough clinical effect, the maintenance dose can be increased to 300mg monthly. After receiving Sublocade 300mg, the average steady state concentration was 6.54ng/mL, and with 100mg the average steady state concentration was 3.21ng/mL. According to the Sublocade Clinical trial, the reduction of illicit opioid use disorder was associated with plasma concentrations of 2-3ng/mL and mu-opioid receptor occupancy of ≥ 70%.3,4
Serum concentrations with transdermal buprenorphine (Butrans) 10mcg/hr (240mcg per day) with multiple doses were 0.224 ng/mL. 5 Buccal buprenorphine(Belbuca) dosed at the same 240mcg per days dose (as 120mcg every 12 hours) resulted in serum concentrations of 0.364 ng/mL +/-0.125.6 With sublingual buprenorphine/naloxone(Suboxone) 8/2mg, serum concentrations of buprenorphine were 3.37 ng/mL +/-1.8.7
In the United States, the max dose of transdermal buprenorphine is 20mcg/hr. It is capped here due to possible QTc prolongation, as studies of 40mcg/hr resulted in clinically significant increases in QTc.5 However, Suboxone and other formulations used for opioid use disorder are approved for dosing much higher than those approved for pain. In Europe, transdermal buprenorphine is available in 35, 52.5, and 70mcg/hr patches to be changed every 4 days.8
Sublocade comes with a warning to avoid use in patients with possible risk for prolonged QT interval or cardiac disease due to a phase 3 trial in which 7 of the 404 patients experienced an increase in QTc more than 60 ms, with one of these patients reaching a QTc of more than 500 ms. It is noted that these findings were sporadic and transient, and no patient experienced an arrhythmia.3
The ability to use a once monthly injection administered by a healthcare provider could benefit many patients. It would be particularly helpful in patients who are at risk for diverting substances, since the healthcare provider is the one injecting the substance. This also means the patient would be required to have monthly visits with a healthcare provider in order to receive their medication, and the provider would be able to ensure steady serum concentration. Currently, Belbuca(buccal buprenorphine) and Butrans(transdermal buprenorphine) are approved for use in pain management. Using Sublocade for pain would allow patients who are unable to use Butrans or Belbuca to continue to experience the benefits of buprenorphine, and the compliance would presumably be better. Additionally, patients sometimes experience irritation at the application site of Butrans or even a full allergic response to the adhesive. With Belbuca, some patients are unable to use the buccal films if they do not have in-tact healthy oral mucosa or the manual dexterity to insert the patch on the buccal area as directed. An inability to produce enough saliva can also interfere with the absorption of the buccal film formulation. Sublocade gives these patients another alternative option should buprenorphine continue to be the best option for their treatment. Patients would be able to manage their chronic pain without worrying about taking a tablet daily, inserting a buccal film twice daily, or changing a patch weekly. It would allow providers to ensure steady serum concentrations and give patients a safer treatment option. It allows the same benefits as it does with the treatment of opioid use disorder, so why not allow those with chronic pain to reap these benefits?
And here’s a thought…
For those patients receiving a once monthly injection for opioid use disorder or for pain that live in remote areas requiring 1-2 hours of driving, why not allow community pharmacists to inject the product so that a STABLE patient only has to visit the buprenorphine prescriber once every 3-6 months? Certainly, the pharmacist could evaluate patients and provide feedback to the prescriber. Wouldn’t that help promote buprenorphine use in patients that truly need it? We know that pharmacists are perfectly capable of giving injections in the community setting and counseling patients – but perhaps it is another case of Nobody Knows as seen in an earlier post.
In closing, we must remember that with any extended release receptor blocker, treating pain post-operatively can become quite a challenge, requiring a team approach to assure adequate pain relief and a safe environment prior to and following surgery, especially for patients with an underlying opioid use disorder that may be prone to relapse in the absence of buprenorphine. For a review and important considerations when treating perioperative pain for both elective and emergent surgery, see references 9 and 10 below with provided hyperlinks.
Questions and comments are always welcome!
GUEST BLOGGER Caroline Breen is a 2018 PharmD Candidate at Western New England University College of Pharmacy. She just completed an advanced practice rotation with the multidisciplinary pain team at the Stratton VA Medical Center in Albany NY under the mentorship of Drs. Erica Wegrzyn and Jeffrey Fudin. After graduation, she plans to continue her career as a community pharmacist.
References
- FDA Approves SUBLOCADE (Buprenorphine Extended-Release), the First and Only Once-Monthly Injectable Buprenorphine Formulation to Treat Moderate to Severe Opioid Use Disorder [Internet]. Indivior UK Limited; 2017 [cited 2018 Feb 5]. Available from: http://www.indivior.com/wp-content/uploads/2017/11/SUBLOCADE-FDA-Approval-Press-Release.pdf
- Cleary JP, Gottwald J. A brief review of buprenorphine products [Internet]. Pharmacy & Healthcare Communications, LLC; 2016 [cited 2018 Feb 5]. Available from: http://www.pharmacytimes.com/contributor/jeffrey-fudin/2016/03/a-brief-review-of-buprenorphine-products
- Sublocade [package insert]. North Chesterfield(VA): Indivor; 2017. Available from: http://indivior.com/wp-content/uploads/2017/11/SUBLOCADE-Prescribing-Information.pdf
- Nasser AF, Greenwald MK, Vince B, et al. Sustained-release buprenorphine (RBP-6000) blocks the effects of opioid challenge with hydromorphone in subjects with opioid use disorder. J Clin Psychopharmacol. 2016 Feb; 36(1): 18–26.
- Butrans [package insert]. Stamforc(CT): Purdue Pharma L.P.; 2014. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021306s015s019lbl.pdf
- Belbuca [package insert]. Malver(PA): Endo Pharmaceuticals;2015. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/207932s000lbl.pdf
- Buprenorphine and naloxone. In: Lexi-Drugs [database on the Internet]. Hudson (OH): Lexi-Comp, Inc.; 2018 [cited 2018 Feb 5].
- Transtec 35, 52.5 and 70 micrograms transdermal patch [Internet]. Cambridge: Napp Pharmaceuticals Limited; 2015 [cited 2018 Feb 5]. Available from: https://www.medicines.org.uk/emc/medicine/8839
- Bettinger JJ, Fudin J, Argoff C. Buprenorphine and Surgery: What’s the Protocol? In Kean N, 2nd ed., Opioid Prescribing and Monitoring—How to Combat Opioid Abuse and Misuse Responsibly. Chap. 6. Pg. 73-78. Pub. Vertical Health, LLC. September 2017.
- Fudin J, Srivastava A, Atkinson TJ, Fudin HR. Opioids for Surgery or Acute Pain in Patients on Chronic Buprenorphine. In Aronoff G, ed., Medication Management of Chronic Pain: What you Need to Know. Publication pending, Trafford Publishing, 2017. Book purchase is available HERE.

Can someone tell me what the process of switching from suboxone film (12mg sublingually/ day) to the sublocade shot looks like currently? How/ What is the transition/ preparation?
Hi, I have been on Sublocade for 9 months now, I was the 8th person in Australia to go onto it. My doctors rooms call me usually 2 days before the injection is due and I pay for it in advance. This seems to work well for everybody. He has the injection ready in his office when I go in for my appointment. I find the injection to be extremely painful, often I have to sit in the car for about 30 minutes until the pain settles before I can drive home. I have stayed on the 300mg dose as the 100 just didn’t cover me for the full month. I am having the injection more for my chronic back pain than opioid addiction. When I started on Suboxone and Subutex in hospital it relieved my pain so much that we decided to try the Sublocade, and it has improved my back pain so much that after 2 1/2 years I am now back at work full time. The biggest problem I have is the lumps it is leaving in my stomach. I now have 9 and they are not going away. Some of them are quite painful to touch. My doctor has about another 10 patients on it and seems pretty dedicated to providing this treatment option.
Jackie, Thank you for sharing. Are you able to get Probuphine in Australia? If so, it might help avoid the “stomach lumps”.
I’m wondering after you have the third shot of 100 mgs and you have withdrawals and they find your levels not right what is the next step? Going back to 300 mg.?
I would leave the dose and add clonidine.
Yes you could go back to 300, depending on what your doctor says.
Hi Jeff,
I have been doing research on Sublocade and stumbled accross your article. You seen well educated in it and unfortunately because it is so new there is little information about it besides on the drugs website (whose bias I am skeptical of) and wanted to ask your opinion. I just enrolled in an Outpatient program offering a 3-5 month Sublocade program with weekly groups and therapy. I am 26 and most recently I took methadone for maintenance and went from 30mg to 100mg over 3 months, and stopped cold turkey after moving and insurance failing. I went to a detox and last took methadone 25 days ago BUT started with the outpatient on sublingual Suboxone induction for 2-3 weeks until shot is covered and ordered.
Many Sublocade providers (including my new program) are stating there have been multiple signs of NO withdrawal after receiving x1 300 mg injections for 2 months and a final 100 mg injection, and I would rather do only 3-5 months on it but also combined with 12 steps and therapy. I do not want long term or life time on this drug as that alone has not worked for me, but I do need help with initial first months of cravings with an end goal of zero buprenorphine, because relying on a drug for a lifetime changes my mindset to inevitable drug seeking (I.e. eventually relapse on other RX meds like benzodiazepines which when mixed have given me disastrous results). However I do not want to experience withdrawal as this will drive me to cravings and eventually usage. My questions are this:
1) How likely am I to have withdrawal symptoms when the drug is so delayed release with a drug that already has a long halflife?
2) Are my programs claims that this is a slow enough taper accurate in your opinion?
3) How long will I test positive for buprenorphine on a UA test?
4) Is there a way for a lab test UA to show decreasing levels?
I appreciate your help and hope this method of reaching out is okay. I have had over 20 attempts at detox / treatment, I’ve tried vivitrol, methadone, and Suboxone maintenance, I’ve tried 12 steps alone, and anything you could probably think of to stay off intraveous heroin over the past 10 years. Any input would be beneficial and life saving, as I’m trying to move forward and make the decision for myself without becoming dependent on something else.
Thank you so much for your time and any potential advice.
Hi Jeff,
I have been doing research on Sublocade and stumbled accross your article. You seen well educated in it and unfortunately because it is so new there is little information about it besides on the drugs website (whose bias I am skeptical of) and wanted to ask your opinion. I just enrolled in an Outpatient program offering a 3-5 month Sublocade program with weekly groups and therapy. I am 26 and most recently I took methadone for maintenance and went from 30mg to 100mg over 3 months, and stopped cold turkey after moving and insurance failing. I went to a detox and last took methadone 25 days ago BUT started with the outpatient on sublingual Suboxone induction for 2-3 weeks until shot is covered and ordered.
Many Sublocade providers (including my new program) are stating there have been multiple signs of NO withdrawal after receiving x1 300 mg injections for 2 months and a final 100 mg injection, and I would rather do only 3-5 months on it but also combined with 12 steps and therapy. I do not want long term or life time on this drug as that alone has not worked for me, but I do need help with initial first months of cravings with an end goal of zero buprenorphine, because relying on a drug for a lifetime changes my mindset to inevitable drug seeking (I.e. eventually relapse on other RX meds like benzodiazepines which when mixed have given me disastrous results). However I do not want to experience withdrawal as this will drive me to cravings and eventually usage. My questions are this:
1) How likely am I to have withdrawal symptoms when the drug is so delayed release with a drug that already has a long halflife?
2) Are my programs claims that this is a slow enough taper accurate in your opinion?
3) How long will I test positive for buprenorphine on a UA test?
4) Is there a way for a lab test UA to show decreasing levels?
I appreciate your help and hope this method of reaching out is okay. I have had over 20 attempts at detox / treatment, I’ve tried vivitrol, methadone, and Suboxone maintenance, I’ve tried 12 steps alone, and anything you could probably think of to stay off intraveous heroin over the past 10 years. Any input would be beneficial and life saving, as I’m trying to move forward and make the decision for myself without becoming dependent on something else.
Thank you so much for your time and any potential advice.
Sincerely,
Blake from Los Angeles, CA
Blake,
Here are the answers to your questions..
1) How likely am I to have withdrawal symptoms when the drug is so delayed release with a drug that already has a long halflife? Not likely
2) Are my programs claims that this is a slow enough taper accurate in your opinion? Yes
3) How long will I test positive for buprenorphine on a UA test? Could be up to 1-month after stopping sublocade
4) Is there a way for a lab test UA to show decreasing levels? If it’s a chromatography test, it can show a downward trend in concentrations, but that is not the most reliable method. It’s best to monitor this via blood levels.
Thank you for your help, I greatly appreciate and plan to move forward with getting the shot.
Good luck to everyone in finding the right solution for themselves.
You have to have controlled relief on suboxone for at last 7 days before you can even begin the process of getting this medication, also you can not go to your normal pharmacy to pick this medication up, only these special pharmacies have them and they call you to ok delivery to your doctor and then it is delivered to your doctor, also not every doctor is qualified to give these shots
Hello,
I’ve recently begun using Sublocade in lieu of Suboxone and really feel like it’s been life changing. That said, I am also working towards having bariatric surgery (sleeve) and am concerned about the surgeon being ok with the fact that Sublocade is in my system. My prescribing doctor is open to working with my surgeon, but I wanted to know if you have any thoughts about this.
Allison, You need to be up-front with your surgeon for safety reasons, if nothing else. There are several ways to handle this. My preference would be IV buprenorphine for pain following surgery. See the following…
Bettinger JJ, Fudin J, Argoff C. Buprenorphine and Surgery: What’s the Protocol? In Kean N, 2nd ed., Opioid Prescribing and Monitoring—How to Combat Opioid Abuse and Misuse Responsibly. Chap. 6. Pg. 73-78. Pub. Vertical Health, LLC. September 2017.
Fudin J, Srivastava A, Atkinson TJ, Fudin HR. Opioids for Surgery or Acute Pain in Patients on Chronic Buprenorphine. In Aronoff G, ed., Medication Management of Chronic Pain: What you Need to Know. Trafford Publishing, 2017.
I have been on norco 10s 325 for about 4 yrs. I have weaned myself down to 2xs a day. My dr. Wants to put me on belbuca 75 strips twice a day and I am hesitant. I am 65 yrs old and take morphine prn 15mg Er . I only use that maybe 2 or 3 times a month. My pain is from back fractures and arthritis. I am afraid of the 12hr strip. Could this benefit me? I do have copd and heart failure that is under control. Afib. I take metorprol 50mg once a day and two water pills and 20mg of xraelto at dinner.
Nancy, Since this is a complex case requiring careful attention and medical advice, please send me an email to jeff@paindr.com. For now though, I will say that extended release morphine (or extended release anything) should never be taken “as needed”.
My boyfriend received his first injection 11/19/18 of sublocade 300 mg. We have been excited about this possibility of a monthly injection for 2 years but there was none approved with the insurance. We have had numerous difficulties for 2 years getting the monthly prior authorization of suboxone, & ready to do anything to ensure he isn’t left with no treatment- as many of you know – he cannot be on nothing.
The injection site has a 6 inch red warm indurated area with a depot just bigger than a half dollar. I’m wondering if it was administered properly. He has been on bup SL tab 16 mg/day which controlled his symptoms fairly. The suboxone film worked much better than the buprenorphine alone. The insurance would no longer approve the films and we can not afford to buy them. Requiring an increased amount of Xanax to aid with the overt anxiety of going through withdrawal when we cannot afford the medication.
He has continued taking 8-12 mg/ day SL since receiving the injections as directed.
He is clearly having symptoms of withdrawal including the runny/stuffy nose, watery eyes, itching of every part of his skin, lack of appetite, no energy, pain, anxiety, restlessness, gi disturbance, and changes in personality- appearing to look “high”.
He is well versed and knows when he is feeling withdrawal symptoms after 18 years of opiate use/abuse. I am a Critical Care nurse of 24 years and clearly see he is withdrawing.
So far the sublocade does not appear to be effective, and I’m seriously questioning the injection site appearance along with the symtptoms of withdrawal. Is there a plasma test available in a regular lab? Or urine?
He was the first patient to receive this injection from his physician. I am hopeful that after 7 days this may subside, but I am a realist and I can clearly see the difference.
If anyone has any suggestions please advise.
Yes. A serum buprenorphine level can be done and the area should be evaluated for infection as that could affect absorption of drug.
Why such symptoms of withdrawal? It seems it should be more effective .
Lisa, It is very complex to explain and requires a keen understanding of pharmacology and stereochemistry for a full explanation. In short though, a pure single action full agonist with only mu activity such as oxycodone or morphine have the typical opioid effects such as analgesia, respiratory depression, euphoria, suppression of noradrenaline (causing drowsiness at first until tolerance builds as the brain starts making more NA to compensate), and additional activities. Buprenorphine has a higher binding capacity for the mu receptors which disallows drugs like oxycodone to occupy mu receptors. But buprenorphine does not have the same effect on NA in the brain when occupying the receptors in favor of oxycodone. While the analgesic activity can be the same or better with buprenorphine, now there is excess NA that was adjusted upwards due to the oxycodone. That causes withdrawal symptoms which are similar to what you would see if you injected epinephrine or norepinephrine (aka noradrenaline). Until the brain resets the NA, there will be some withdrawal symptoms.
I’m a Crit nurse also with lots of Sun experience
I will say with 300 mg in a depot and him taking 24 sl also at same time
he may be getting too much bup I’ve seen withdrawal like symptoms when too much is taken becomes
revolving battle for the receptor site and when u add the Naloxone sl to it while I get the absorption is minimal ect ect I still believe there is more then u think but lower affinity is
not making it beet bup off Miss you receptor
Spell check and in car excuse sp
Bottom line think maybe cut back on sl bup while 300 depot in
May c decrease in symptoms of withdrawal like
I am a pharmacy student and have been reading about this medication for the past week or so. The benefits of having a long acting form of the medication are clear but I am wondering how would we taper a patient off of this type of medication or if the manufacturer has any data on this. I have had a few patients ask me how they could transition off the medication if at some point in the future they wanted to, under the supervision of a healthcare provider of course. The patients I spoke with were asking mostly if they would have to go back to a different form of buprenorphine and then taper off of that.
Michael, This is very valid question. I will paste important information from the package insert below, which I’m assuming you’ve read. However, to get to the point of your question, the following passage in the PPI is perhaps most relevant. “Initiating treatment with SUBLOCADE as the first buprenorphine product has not been studied. Initiate SUBLOCADE treatment only following induction and dose‐adjustment with a
transmucosal buprenorphine‐containing product [see Dosage and Administration (2.4)].” As such, discontinuation should occur the same way, that is, by monitoring the patient, and if supplemental buprenorphine is needed, a SL dosage form could be used to taper.
2.5 Clinical Supervision
Periodic assessment is necessary to determine effectiveness of the treatment plan and overall patient
progress. When evaluating the patient, examine the injection site for signs of infection or evidence of
tampering or attempts to remove the depot.
Due to the chronic nature of opioid use disorder, the need for continuing medication‐assisted treatment
should be re‐evaluated periodically. There is no maximum recommended duration of maintenance
treatment. For some patients, treatment may continue indefinitely. If considering stopping treatment,
the clinical status of the patient should be considered.
If SUBLOCADE is discontinued, its extended‐release characteristics should be considered and the patient
should be monitored for several months for signs and symptoms of withdrawal and treated
appropriately. After steady‐state has been achieved (4‐6 months), patients discontinuing SUBLOCADE
may have detectable plasma levels of buprenorphine for twelve months or longer. The correlation
between plasma concentrations of buprenorphine and those detectable in urine is not known.
Risk of Opioid Withdrawal With Abrupt Discontinuation: If treatment with SUBLOCADE is discontinued, monitor patients for several months
for withdrawal and treat appropriately. (5.8)
Risk of Withdrawal in Patients Dependent on Full Agonist Opioids:
Verify that patient is clinically stable on transmucosal buprenorphine
before injecting SUBLOCADE. (5.11)
5.8 Risk of Opioid Withdrawal With Abrupt Discontinuation of SUBLOCADE Treatment
Buprenorphine is a partial agonist at the mu‐opioid receptor and chronic administration produces
physical dependence of the opioid type, characterized by withdrawal signs and symptoms upon abrupt
discontinuation. The withdrawal syndrome is milder than that seen with full agonists and may be
delayed in onset [see Drug Abuse and Dependence (9.3)].
Withdrawal signs and symptoms were not observed in the month following discontinuation of
SUBLOCADE. Considering the long half‐life, any withdrawal signs and symptoms that may occur would
be expected to be delayed [see Clinical Pharmacology (12.2)]. Model simulations indicate that steady‐
state buprenorphine plasma concentrations decreased slowly over time following the last injection and
remained at therapeutic levels for 2 to 5 months on average, depending on the dosage administered
(100 or 300 mg, respectively).
Patients who elect to discontinue treatment with SUBLOCADE should be monitored for withdrawal signs
12
and symptoms. Consider transmucosal buprenorphine if needed to treat withdrawal after discontinuing
SUBLOCADE.
Do you think dropping injection dosage to 50 then 25 along with allowing for intrinsic slow taper
would aide patients I feal once they go back on SL bup we ll
just circle around and end up not getting them off
This is for the group that can’t manage WD only.
I also think post DC at 3-5 or 12 months starting Viv /naloxone inject is best goal soon as acute WD s are over and Paws start
But with such long half lives I’m concerned relapse levels will be high or Viv will induce severe acute WD s bc bup still in depot 12 later
Maybe a quick full agonist taper even in patient may work in end
I think this is a wonderful thing if it works! Would cut down on overdoses, people buying and the sale of their opiates. I’ve been on Methadone 30mg for 8 years now for chronic pain because it was the cheapest I could buy since I had no insurance and needless to say I can’t tell it really does anything now! I had gastric bypass surgery 14 years ago and another lady I know also had it and told me that with the surgery we didn’t absorb any meds in needed quantities so I wonder if I even absorb the whole 30mg? Can anyone answer that for me!
Generally this will not reduce methadone absorption.
carlaj0604@gmail.com
The side effects of this sped-to-market medication (2-trials, 24-weeks) were minimized, and that’s showing in the mixed bag of efficacy being reported on many sites and blogs. So many stories of major, sudden physiological withdrawals that hit patients hard.
My insurance company actually approved me for Sublocade last week, without me knowing it (I was denied in February), and my doctor was beyond excited to TELL me last month when I showed for my monthly appointment. A little too excited, actually, which made me question his motives, so I flat out, directly asked him, “Dr. A, what type of incentives are you receiving from the company representing Sublocade?”. He paused, looked at his computer, and sidestepped my question and replied, “now, why would that be the first thing that comes to your mind?”. He then proceeded to ask about my blood pressure medication and whether I was following through with my 12-Step & SMART Recovery schedule we agreed to (I am), and entirely ignored my question. I let it go. No bigs.
Ultimately, when I refused the shot (which was already on the table, fresh from the fridge), he threatened – er, “suggested” – we begin an immediate taper of my generic bupe/nax (8/2=16mg/day) that month. He was agitated & fidgety (I’ve known him for nearly 2-years). I remained calm. He reminded me that he “ordered that injection specifically” for my visit.
I asked if I could make a suggestion, and he agreed. I kept my cool and said, (paraphrase, though I’ll use quotations because it’s first person) “Dr. A., I like the idea of Sublocade. At this point, I don’t feel comfortable with moving away from what has been working so well. Thank you for caring enough for me to consider me as your first Sublocade patient. I would like to have a more detailed discussion about switching at my September appointment. Until then, we can both continue to research the efficacy of this brand new medication.”
I predict this medication will be a disaster and pulled from market for lack of profitability/market share, that is already coming via word of mouth from about half the patients being injected.
Doctors have concern (they should) about patient diversion. I have one friend who’d doctor requires him to bring in his entire script of 60 Suboxone Film wrappers each month. The same doctor does “spot” UA’s. You get a call and are required to come in a offer a sample within 48-hours. She says she asks this of her patients to ensure compliance for the entire month.
Sublocade aside, I like the Sub Film because I’m in the process of tapering off. I get a script for 8/2’s and trim it 6mg. Next month I’ll be cutting them in half and seeing how I respond to 4mg (8 mg a day). Yes, my doctor knows and this is how we are managing my taper schedule.
Finally, Suboxone is more effective for pain than all the Fentanyl and Oxycodone my doctor had me on for 2 years, that I knew my body was gripped to and I wanted off of it. I had no idea what a floating zombie I was when I was on all those narcotics. I’m now present in my loved ones lives.
Thanks for this article, Doctor. I appreciate the opportunity to participate in the discussion.
In my experience, side effects to buprenorphine are most often seen when a patient continues to use a full agonist opioid such as methadone, oxycodone, morphine, etc. When these continue to have a presence, the side effects are generally refelctive of opioid withdrawal, not buprenorphine itself.
I agree, and even though it’s inconsequential to my post, it’s a critical point to make, If a person is taking Bupe as part of their monthly “spin cycle” routine, to adjust their tolerance and eat a few good meals, well, then that’s a recipe for disaster that can only work for so long.They’re the type of patients who are difficult to engage because they’re unable to reliable in reporting. You need to be 100% honest with your doctor, even is the conversation is difficult to have>
I had to reply I just started the sublocade injection two weeks ago worst mistake I’ve every made doing great in my recovery thank God or I would of fell off already due to the out of the blue painful withdrawn symptoms I’ve been having so frequently sometimes at midnight sometimes after work sometimes first thing in the morning but just to share my expierence I had to say something I went to the doctor last week she gave me a script for two half 8 per day to use to supplement the missing dosage still not feeling well atleast the sublocade works for 12 out of every 24 hours though rummaging for that much
I think we may be underestimating the cardiac risk of buprenorphine, eg prolonging QT interval. As a practicing Pain Medicine specialist, I altered my methadone prescribing significantly when I became educated about methadone effects on cardiac conduction. I will be very cautious with buprenorphine especially in patients with any other risk factors. Believe baseline EKGs should be performed prior to initiating treatment with buprenorphine as we do with methadone, but I know that’s unlikely to happen.
Dr. Weinstein; Thank you so much for this important insight. I haven’t seen an issue yet, but I am careful about doing baseline EKGs up front as you suggest. I agree that caution is especially important when injecting a once monthly dosage form.
I’ve seen TDP come in initially missed as a seizure but then strips
run b4 after events in patient showed qt interval issue
ESP when u add anti depressant s which’s really common and some muscle relaxers like Robaxin
to mix I ve seen cardiac issues dev that missed at seizures at first.
When u have a common Pharm profile of a Opiatr abuse dx anti depressants and non narc alternatives to pain mgt are common
Funny thing is even in presence of Gabbapent dx mjssed and given seizure new onset
Did some personal research. Found a mixed picture where it comes to Buprenorphine as an analgesic:
“Analgesic Properties of Maintenance Opioids:
Patients receiving maintenance therapy with opioids for addiction treatment do not derive sustained analgesia from it. Methadone and buprenorphine, potent analgesics, have a duration of action for analgesia (4 to 8 hours) that is substantially shorter than their suppression of opioid withdrawal (24 to 48 hours). Because most patients receiving OAT are given a dose every 24 to 48 hours, the period of even partial pain relief with these medications is small.”
Source (2006): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1892816/
It seems that a constant-infusion system would need to maintain relatively high plasma levels in order achieve continuous analgesia(?). This in addition to the known strong competitive inhibition with other (endogenous as well as exogenous) Mu Opioid Receptor (which includes 100 or so variants) agonists – causing potential serious dilemmas in acute injury with accompanying severe pain situations. Ketamine ?
.
As well, for N40D variant patients, these findings may be relevant where it comes to analgesic efficacy:
“We found that the N40D variant had a negative effect on the signaling of the commonly prescribed opioid buprenorphine in all of our assays. … The N40D variant did not affect signaling of any of the other 10 opioid ligands tested, including β-endorphin. … Buprenorphine is commonly prescribed as both an analgesic and as an alternative to methadone for the treatment of opioid dependence, and differences in signaling arising from the N40D variant may be of clinical significance.”
Source (2014): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4241093/
“… data suggest that the OPRM1 A118G SNP will significantly impact the clinical efficacy of BPN in its therapeutic applications.”
Source (2017): https://www.ncbi.nlm.nih.gov/pubmed/28188737
.
Some possibly interesting research lately positing endogenous opioidergic systems in many aspects of being human (wanting, liking, social responses, etc). Have been wondering if (and if so, how) the central and peripheral neurological “terrain” is able to bypass, and in some manner(s) functionally replace, the ubiquitous Mu opioidergic systems being subjected to long-term continuous blockade from all agonists.
I think many patients who became addicted to opiates post bariatric surgery ended up on bup very fast
Early in addiction length
By nature they seek fast fix and started
Bup to stop percs bup became drug
Of choice
Long Food addiction – oxy 6-12 months – long bup addiction / Maintenance
They end up regain weight in bup maint period
I think addiction and circular nature of it
when never treated w psychological comp ends up dealing moral with Pharmco issue u express.
No real data nurse for 39 years in Crit setting w large opiate dependent pop
And bariatric surgery and new onset opiate addiction is anecdotal thing I think I’m seeing and mentioning
No data to support possible study
Use OPRM1 A118G SNP study
as support for neuro bio basis for psychsocial issue
Is Buprenorphine really the best pain killer for those in sever, chronic , intractable pain like CRPS, type 2, Stage 4? I have been on methadone for pain, successfully, for a decade. I compromised with methadone because I don’t like the addled feeling I got from other opiates, fortunately, its been successful in controlling my pain, although I’m never not in pain. Even on methadone. For a decade, I had a prescription for 90 mg/day of methadone, of that I would usually only take 70 or 80 mg/day. Last year, as they force tapered everyone, I lost 47 lbs. and couldn’t eat or sleep due to intense, unending, unremitting pain. I thought about putting a bullet in my head many times, particularly in the middle of the night, as I was writhing in too much pain to sleep, or eat, or read, or anything. As the forced tapering dropped below the level of a therapeutic dosage for pain, for me around 40 mg/day, I started to rapidly lose weight and could no longer sleep due to the unmitigated pain, and it just got worse as the tapering continued. I begged to be referred to a specialist, whom I had seen in the past, a specialist in Complex Regional Pain Syndrome, at a nearby teaching university, with a world-famous pain clinic. He recommended immediately increasing my dose back up to a therapeutic level. My new primary pain doctor, in my county, as of January, last year – who’s only mandate it would seem, was to indiscriminately force-taper everyone off of opiates – was either too stupid, or too arrogant, to agree with the specialist and continued the forced tapering.
Fast forward six months. I now drive 30 minutes, each way, each morning, to a methadone clinic, and since I now only have one, monolithic dose in the morning, its much higher than it ever has been. As a final note, I tried Suboxone years ago and it did little, to nothing, for my pain. I’ve considered moving to another country, one that actually care about their patients; becoming an ‘opioid refugee’, but I lack the funds for that.
It’s no surprise to me that buprenorphine was inferior to methadone for CPRS. The reason is that unlike buprenorphine, methadone blocks NMDA receptors which specifically help with neuropathic pain. Perhaps your doctor would consider levorphanol which has similar activity to methadone but has many advantages over it.
What happens when someone develops a tolerance? My brother had his pain effectively treated with Butrans Patch. The patch was helpful as late as last August but now he is suffering again. The addition of percocets don’t seem to be making much of a difference. Any information wold be helpful. Thank you
Percocet won’t likely work well while on Butrans. He should speak to his doctor about transitioning over to Belbuca.
I live in Albany NY.I been clean for over 6 years now.Im currently taking 48mg of Suboxone a day. I’m trying to get off this medication but the withdrawals symptoms are to much. Due to the job I have I can’t just go to a rehabilitation Center and Detox for 30 days or more,I have responsibilities and people that depend on me to have an income. I try to talk to my Dr when I found out about Sublocade and even my insurance covered it. But my Dr is giving all kind of excuses to not order the medication. He said that the office can’t afford paying for the medication up front even when he knows the insurance will refund I’m the money. I’m desperate because I want my life back plus my job can drug test me at anytime and I will loose my job.And that will be my end and my family as well. Can anyone help?Does anyone knows about a Dr in Albany NY that is doing Sublocade injections?Im scared.I really think that Sublocade can help me tamper down on dosage so I can be finally free.Does anybody have answer for me?
I would find another doctor. I will send you a separate email.
My question is this.. What about patients who are unable to take long acting medications, or who are rapid metabolizers? Is this medication going to be the turning point for ALL who take oral opioids? Many like myself have a very hard time finding the right medication that actually works for them due to major sensativity issues. From everything I’ve read in the last few weeks, it seems that big pharma is trying to get rid of oral opioids which leaves thousands of legit Intractible pain patients like myself with little to no options due to our genetic makeup.
Why is no one addressing this situation? No two people are alike and it seems that Dr. Fudin is the only one who has spoken about poor and rapid metabolizers in patients. This needs to be addressed more so physicians can be aware that it is a real problem for patients.
Dr Fudin here is a huge help. I’ve handed
dr s his printed pages and articles from his site
Sadly best thing u can do is just keep looking for best doc you can find.
You will get him or her eventually
I ve found often if your truely not abusing you ll be able to get a doc to listen
This med not for everyone SL bup not going away bc insurance not covering SBLC but the med has a lot of up side for those it works for.
I was put on opiates I had a “good doc”
He wrote more and more I knew the deal
I did have pain issues but opiates are addictive I never had an addiction in my life they got me I was out on suboxone just as fast and that’s sooooo hard to stop. The half life combined with the peak trough add the active norbup metabolite. Weening it down the way you need to and remember by now your addicted u have misused to cope even if it was only few times.
So we all know Sub SL a life sentence
I was middle age no hx abuse I have money job family help with any isssue I needed and got hooked I should have been able to walk away but it s hard
The weening is the part this drug brings to the table slow wo the ability to use it to cope.
I’m on it a month and I will say it’s great
I plan to do fewest injects studied
but will never go back on bup sl
This drug is not for everyone
This Fluidcrystal tech cam2038 depot is not as new as it seems and Bup is not new
It’s the combo that’s new.and def not for everyone. But being on both sides of fence I chose to do it and I’m happy I did
I’m hoping I get the slow ween they report. I took my whole profile and looked at inducers and inhibiting meds
I did everything I can to mace sure it
acts as depot data suggests.
Let’s hope it does
I did get cardiac work up prior bc of worries I have w QT interval issues
And I stopped meds that also caused issues. I have no planned surgeries and hope to be done w Sub in two years at most bc of this med
Not for all not for you maybe but I think it brings so much to table
Pain mgt wise I def saw increase pain first week 3 days only and 3 week I managed it w NSAIDs low dose though
acupuncture hydrotherapy tens unit
I did it all it was more work the taking a film but that’s the coping part w bup
SL and why ithis works for people like me at least I hope
I’m an RN who s been on Bup for 9 years
I have critical care and detox psych background I also worked neuro ICU
BUT anything here is a opinion of the
addict on bup not the RN.
I love this blog I hope I can add to it.
Coming out as a addicted medical professional is very hard but insight you gain is amazing. While I still remain anonymous here I hope one day to not be and addiction be less of a stigma
bc it can happen to anyone if it happened to me .