For many years I was an internist, addiction medicine doc, and specialist in medication management for chronic pain. Around this time of year, when patients were in the “donut hole” of their medical insurance and now had to pay out of pocket for their own medications, I used to spend a lot of time converting some of them from whatever expensive opioid they were on – OxyContin®, MSContin®, OpanaER®, etc. – to methadone. Towards the beginning of the next year though, most were happy to get back on their original drug. I was willing to do this because it was the only way they could continue getting relief from their legitimate pain. But it meant a lot of extra work for me.
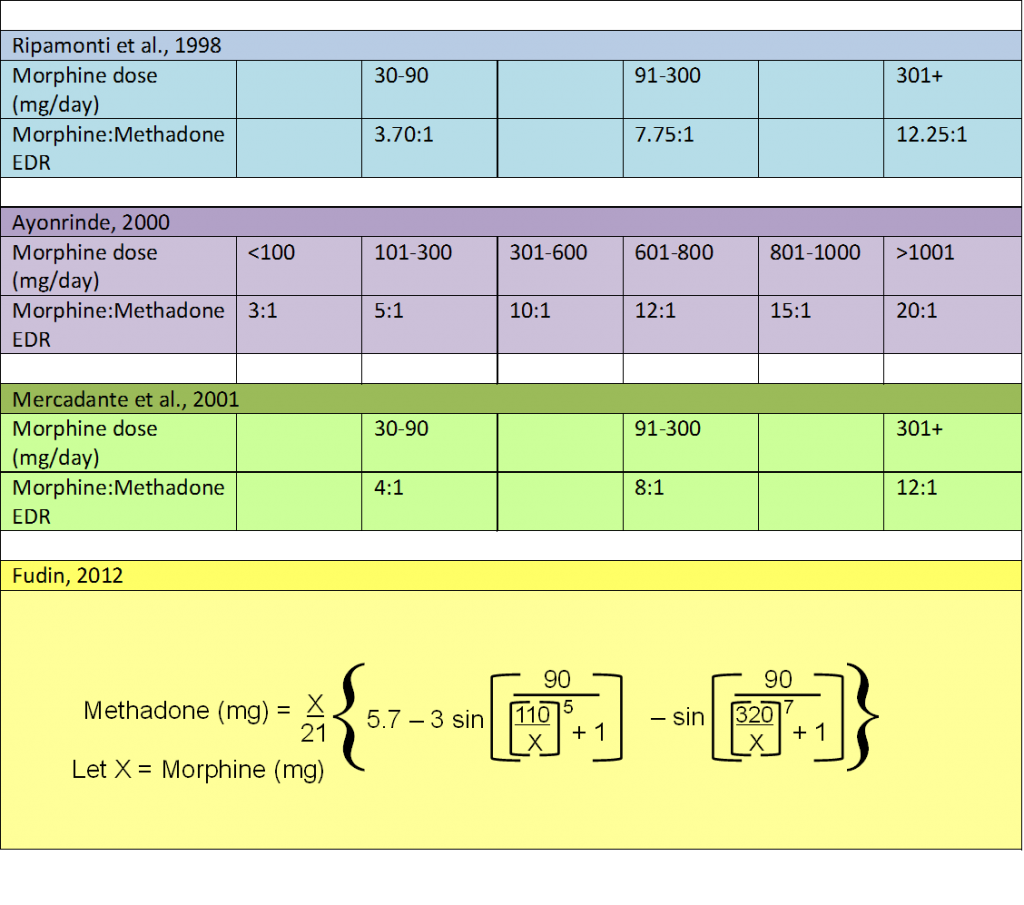
Switching between most opioids simply means knowing the conversion ratio. (and initially, reducing the new drug by about 50% of the calculated equivalent to minimize the risk of overdosing). For example oxycodone is generally 1.3 to 1.5 times as potent as morphine, so that 15 mg of morphine is equianalgesic to 10 mg oxycodone; 60 mg of morphine is equianalgesic to 40 mg of oxycodone; 300 of morphine is equianalgesic to 200 mg of oxycodone. See Opioid Calculator page on this Website. The same is not true of methadone – the higher the morphine-equivalent dose, the relatively higher is the ratio of morphine to methadone. The table on the right shows these ratios in various schematics.1
Dr. Fudin recently developed a mathematical model for calculating this which appears on the Website (Methadone Dose Conversion Unscrambled) and the table herein, but there is still uncertainty for individual patient conversion and significant variations by population due to polymorphic differences. This means more frequent visits and phone calls, longer explanation to the patients about the conversion process, and also dealing with the particular characteristics of methadone.
Methadone is an effective analgesic. It is a synthetic mixture of d- and l-isomers. The d-isomer has NMDA receptor antagonist activity. According to research by Dr. Charles Inturrisi, the d-isomer attenuates the development of morphine tolerance and NMDA-induced hyperalgesia.2 Methadone may be more effective than other opioids in treating neuropathic pain. Because of its very long serum half-life (24-36 and upwards to 60 hours for outliers), a single daily dose prevents withdrawal symptoms, which is why it is historically connected with treating heroin addicts. Of course, the addiction connection sometimes frightens patients when I suggest treating their pain with methadone. There’s also confusion about who can prescribe methadone and for what. According to the FDA, only methadone clinics can prescribe methadone for addiction treatment, but any prescriber with a DEA license that includes Schedule II substances can prescribe methadone for pain (even in a patient whose methadone concurrently treats their addiction). [Online MPA Degrees has an excellent schematic of commonly prescribed medications/pharmacological classes which succinctly clarifies DEA Schedules I through V.] It is important, however, to write the words “for pain” on every prescription of methadone for pain.
Working with methadone can be tricky. The FDA has issued multiple warnings about methadone-related deaths, which usually occur in the first few days of using the drug. In an opioid-naïve patient, any opioid needs to be initiated at a low dose and titrated upwards to adequate pain relief. This gives the patient an opportunity to develop tolerance to the sedation and nausea-inducing side effects, which rapidly resolve (unlike constipation, which persists). With most opioids, whose serum half-life is about 4 hours, the dose can be safely increased within a couple of days (after about 5 half-lives until steady state). If the prescriber allows a few extra doses, generally the patient will become sleepy until the drug wears off. But because of the long serum half-life of methadone, increasing the dose every 2 days (rather than 5-7 days as recommended), will cause accumulation of the drug in the body, with possible resulting overdose and death. That’s why starting methadone requires caution, conservative upward titration, and maintaining contact with the patient. In a patient who is being switched to methadone from another opioid, one way to deal with the risks of upward methadone titration is to transition it in stages, leaving the patient on some of the previous opioid so that they continue to get reasonable pain relief. Doctors Lynn Webster and Perry Fine have addressed this issue nicely in this commentary.
In the past, some patients were referred to me from methadone clinics because they also had chronic back or other pain. (These were patients considered very reliable by the methadone clinic, at a low risk of addiction relapse). Typically, these patients would explain that they had good pain relief in the morning, after their daily dose, but by the end of the day the pain had returned. Why? It’s because despite its long terminal half-life, methadone is not a long-acting or extended release analgesic as with other pharmaceutically prepared agents. The solution therefore is to divide the patient’s daily dose into 3 or 4 doses, often with a slight increase. For example, a patient on 80 mg methadone would be put on 30 mg three times daily or 20mg four times daily.
What about breakthrough pain in patients on methadone? In patients with an addiction history, no matter what opioid they’re on for pain, I prefer not to prescribe an immediate-release opioid such as hydrocodone [Vicodin® or oxycodone/APAP (Percocet®)]. What gives a person a sense of euphoria (or just a “good” feeling) is not the concentration of a drug in the blood stream, but rather the rate of increase of that drug in the brain. This is often the reason that recreational users of marijuana prefer to smoke it rather than ingest it in brownies. Similarly, I believe that Vicodin® or Percocet® are more likely to induce CNS effects compared to sustained-release preparations of the same or other opioids, or methadone, which has stable serum levels because of its long half-life.
I remember that many years ago, one of the first patients I treated with methadone for chronic pain required an unusually high dose – 200 mg/day. (A typical dose for addiction in a methadone clinic is about 80 mg/day, and doses for chronic pain vary widely). The patient insisted that lower doses weren’t helpful, so I slowly titrated upwards. She was taking the methadone for chronic headaches related to a head injury, from which she also had seizures. At around that time, serum methadone levels became available, so I shipped off her blood. To my surprise, her serum level was much lower than expected; she was a very compliant patient, so diversion of some of her medication was not a likely explanation. That’s when I learned that Tegretol® (carbamazepine), which the patient was taking for her seizures, increases the metabolism of methadone, thus reduced its serum level (up to 60%) and its efficacy. Unlike most opioids, methadone has multiple drug-drug interactions, some of which reduce its serum levels and therefore its efficacy, while others increase it. These interactions are due to Cytochrome P450 iso-enzymes in the liver that are responsible for metabolizing methadone and many other drugs that undergo similar metabolic pathways. So the prescriber needs to know every other drug the patient is taking and whether that drug interacts with methadone. See Treatment of Neuropathic Pain: the Role of Unique Opioid Agents and Drug Interactions Among HIV Patients Receiving Concurrent Antiretroviral and Pain Therapy. Both are listed on the Resources/Suggesting Readings section of this Website.
One other potential problem with methadone is that high doses can affect cardiac conduction, lengthening the Q-T interval on the EKG and potentially inducing a fatal arrhythmia, torsades de pointes. This is uncommon, but just to be sure, I would get an EKG in patients who were on 80 mg of methadone per day or more. I can say that I never saw a case methadone-induced of Q-T prolongation, but such cases have been reported. EKG’s should be obtained on any patients who receive methadone if they have a family history of Q-T prolongation or if they are on other medications that prolong Q-T interval, especially tricyclic antidepressants.
In summary, methadone is an inexpensive very effective opioid analgesic, but its use requires knowledge of its particular characteristics. I prescribe it often in my practice and it can be used in patients who have the dual diagnosis of pain and substance abuse disorder; but in the latter case it must be made explicitly clear in the record that it is being prescribed for pain.
References:
- Fudin J, Marcoux MD, Fudin JA. Mathematical Model For Methadone Conversion Examined. Practical Pain Management. 2012 September; 12(8): 46-51.
- Note: Although this article is marked “Copyrighted”, a free copy is available at http://www.minervamedica.it/en/journals/minerva-anestesiologica/article.php?cod=R02Y2005N07A0435. Additionally, since NIH, a government agency was involved in funding the research and article “Pharmacology of methadone and its isomers”, certain Copyright laws allow public access and may notg apply. Please review these prior to distribution or reproduction.
Jennifer P. Schneider, M.D., Ph.D., is a physician certified in Internal Medicine, Addiction Medicine and Pain Management. She is the author of 9 books and numerous articles in professional journals. She is a compassionate professional committed to educating others in her fields of specialty. She is a nationally recognized expert in two addiction-related fields: addictive sexual disorders and the management of chronic pain with opioids. Aside from her own practice, her professional activities include writing; lecturing at conferences; serving as an expert witness in legal settings; and appearing as a media guest on television and radio.


Hi. I’ve been a methadone patient for almost two years now, and something that scares the hell out of me bas been happening to me for quite some time. I get excruciating pain spikes in my major joints on a regular basis (ankles, knees, hips, wrists, knees and shoulders, sometimes fingers and toes too) and it’s been getting worse and worse as time goes by. A few days ago I woke up at 3am in a lot of pain and couldn’t go back to sleep, so I got up and got ready for work, toughing out the pain. I managed to get to my clinic, although it was difficult to drive in that much pain, I took my dose, then I made it to my usual parking spot before work. By the time I’d gotten there the pain was so bad that tears were streaming down my face and I had to stifle a scream. I couldn’t control my arms and legs- I was in too much pain to stay still. Then I woke up. 20+ minutes had passed- I’d completely blacked out. I was lucky that I’d been there early or I would’ve been late for work. This has happened before- several times, and I’ve been to the Emergency Room 3 times over it. They thought it was alchohol withdrawal, and the medication they gave me (Adavan) seemed to help quite a bit. They also prescribed Lyria to take home with me. I had assumed that they were right, so I stopped drinking. However, I’ve been sober from alchohol for over 2 months now and this is still happening to me. Every minute of every day, I’m in pain. Not as much as the occasion I described above, but that level of pain is not uncommon for me either. Usually happens in mornings or at night. I’ve spoken to other patients at my clinic as well as some of the staff there and nobody else seems to be having the same problems. One of the other patients mentioned that methadone “seeps into your bone marrow”, and that “by then it’s too late”…. I tried to ask what he meant- too late as in you’ll always be in pain? Or that you’ll die? But he was being called in to take his dose, so I didn’t get a chance to speak with him further about it. I think that there is some other factor besides the methadone, such as some sort of arthritic condition or something else that is causing the pain to begin with, and that when the methadone wears off, it amplifies the pain from whatever the heck type of arthritis I might have… I have a wife and a kid to provide for and can’t miss work to get help- not yet at least- but if there is anybody at all that might have some insight as to what is happening to me, I desperately need to know. Any advice helps.
Great articles
My name is Jeff I’m from Michigan suffer chronic until your body pain for 5 or 6 years now due to an autoimmune condition that was originally thought to be paraneoplastic syndrome but now is considered ill-defined. My paraneoplastic antibodies have all but disappeared as of my last test fingers crossed and they changed my diagnosis to central pain syndrome for lack of a better explanation. I’ve been in every pain killer known to man and none of them worked. The only thing that is work for me as methadone I take 60 grams per day 20 G morning noon and night basically.
Before being treated with methadone I was unable to do a damn thing I was couch-bound. I literally could not cross the street to check my mail I live on a rural route and I live on a busy Street with my mailbox being across that busy Street. I have tried to get the post office to move my mailbox but they will not do it seeing as I’m not in a wheelchair full-time.
But I digress
Right now can at least participated life to some extent I have hobbies I work with metal I have a small scale metal shaft and a wood shop in my garage I grow mushrooms is a hobby for me mushrooms are very very good for you and I figured hey you can’t hurt LOL
I don’t know what I would do if I’m unable to be treated in the future I don’t want to go back to being completely sedentary! my insurance company recently turned down my prior authorization for this year and I am very scared. I can’t afford to buy crab know that I am not working. I don’t know how I will scrape the money together to purchase my pain meds. I found out about pharmaceutical coupons like GoodRx with your wonderful alternatives do they cut the price down from medication so dramatically it’s unbelievable. I talked to my pharmacist about this insurance problem and I said maybe I will just start paying cash and using a GoodRx coupon. He stated to me that it is up to the pharmacist if he wants to accept the coupon or not!! I said what? she tried to hem and haw and describe a reason why they could possibly turn down a coupon for a controlled substance when they take that same companies coupons for every other medication under the sun. We have a really big problem in the United States pharmaceutical companies and insurance companies and pharmacist themselves have too much power in too much say in my goddamn life. It should not be up to them!!!!
And then I see this organization that’s basically a bunch of bored housewives did his issues with controlled substances trying to get them illegal eyes pressuring Congress buying off individual congressman with donations that they organized on Facebook excetera excetera excetera. I just absolutely cannot believe the amount the goal that these people have. I’m over 50!!! Being as sick as I am and as immobile as I have become I am not going to live very much longer! That’s just a simple fact of life in these people go out of their way to try and ruin my life? they have no idea what it’s like not to be able to tie your own shoes at 50 years old!! I’m so sick of people meddling can someone in their family decided to abuse drugs. It’s not my problem and not my fault so don’t punish me for it!
And here I am one of a large majority who cannot take any of the methadone drugs. I can’t say it enough oxycontin saved my life as a person with autoimmunes and a inoperable condition it helped bring inflammation levels down also stop where the body had pain from pain. Still what helps one does not help all and that factor is left out, I think for this report it should have been in it or editing does not do justice for what she wants said
My freids,been on 150 of methadone for 20 plus years.Addiction,and pain,,,so i found out my qt time is really bad.So suboxin is a joke to us hardcores.Vancouver bc east van.Hardcore.So theyve put me on kadian.Morphine in other words.Extra extended time release beads as you take once daily.Well 150 juice eqauls 1100 mg kadian.Thats right,11 hundred miligrams daily.And im still a little sick.But i can think,im 10 times more alert,just everything is 10 better.Methadone is garbage and extremely dangerous,for what cause it doesnt make you feel good.Or get high even.Just telling my little journy.Just about croaked stopping meth abruptly.So be careful.
Omg I feel you on that. I’ve been so scared to come of and this time around I’m on it because of a bad infection I caught and the only pain med I could take was nethadone and now I’m going on two yrs of it and just as of last week have started to come down from 80. Last time I stopped I went right to heroin after the second day and started the cycle all over again. This time I’m all set. After my surgery I now have panic attacks and can’t even think about using again and so it’s been a complicated two yrs. I’ve actually had to give up a role for Chicago pd b/c I wasn’t able to notify the clinic in time and not only that, I had heart surgery so it’s bad for me anyway. I’m just bummed and all over the place. I want off this crap but it’s the most nerve racking experience.
Hey my brother said he took 30 mg out of my bottle and put water in n it’s place,the. K have the prick 50 next day wonder how much I really got left in there man? Never again I’m pissed I been on 150 for 15 years
what the hell is Kadian? And why is it better then methadone?
I’m in Australia. I’m astonished and in awe of the amount you people have suffered and how much you all remain so gracious and reasonable about your treatment, some of it awful, some good. I’ve only worked out recently for myself that methadone works better for my pain ( 2 torn shoulders, 1 bicep, car accident 40 years ago, 3 more rips over last 8 years – not much compared to the horror stories here I see) if i divide my dose into 2 a day. I see from here 3 or 4 times a day may be even better, though its down to quite a low dose now, I’m not very big or heavy, 15 / day. I’m trying to get off and find something else, some other way, even though right now pain is near intolerable but higher doses in past never made it that much better, so I’m looking for something else, I’m so tired of the methadone roundabout and the expense. As for the stigma, what can I say? In a way I’m past caring, but also I can’t be bothered with having to explain and educate the people I like and mix with who don’t know about my use and have all the usual sensational misconceptions, I’m just too tired, in too much pain. I’d lose my temper and lose my non druggie friends! But reading all these reports I’m so astonished now that in 30 years no doctor or pharmacist has ever suggested this idea of splitting the dose 2 or 3 or 4 ways over 24 hours, we’ve always just been told we’re not trying hard enough, or using, or something, when we say its not holding us for 24 hours. Now they are all so surprised when I tell them that’s what I’m doing and its working better . We have a lot to learn from you, yet we constantly get told how lucky we are here that we are not in USA with their dreadful medical system. BS. I do know 100mg Fentanyl patches work well for me, got left some by a dead person, but getting Docs to prescribe them – well you’d think i was asking for a licence to eat babies. I have not found the oxys or Endone to help much. Found bad side effects from Tramadol and amitriptiline and Gabapentin and Lyrica type meds, part of cause of one of the accidents, so I steer away from them. But I know other people get good results and tolerate them so that’s good for them. There seem to be a lot of individual differences that can’t easily be explained without heavy duty science and analysis of individual’s biology and that won’t happen here on the cheap. Pity there can’t be more trust in patients assessment of their needs and descriptions of their reactions, but its a vicious circle; distrust by medical profs leads to patient’s needs to lie and manipulate which leads to more distrust. lol. Any better ideas? Happy to hear them. Thanks all of you.
Holy cow… Reading 95% of the comments is enlightening. I was prescribed pain medication for 7 years after a severe motorcycle wreck in my early twenties. My doctor prescribed me enough pain meds to kill a horse, but since we “trust” a doctor and their opinion and extensive “schooling” I took as prescribed. Btw, this doctor was indicted and died in jail awaiting sentencing (if that truly tells you how many lives he destroyed). After so many junkies doctor shopping, corrupt doctors over prescribing pain medications, and pharmacies failing to comply with DEA standards things became too difficult and I decided to start attending a methadone clinic. I had also learned I was pregnant and found methadone to be the best pain medication management for my unborn child and myself. I attended this methadone clinic for two and a half years and NEVER received any take home medications. Although I was always compliant with their rules and NEVER failed a drug test. i was switched around to 6 different counselors in less than 3 months, but the final straw was when the nursing staff at the dosing Windows overdosed me by 60mg on accident for a week straight while I was reducing my medication on a “blind dose”. They didn’t catch it or even notice it until I received a take home for a holiday (for one day) and my medication was incorrect on the bottle. After seeing the physician there and expressing my anger I transferred to another clinic in another county. Now I have SIX take homes, I’ve never been overdosed, and I only go to pick up my medications once a week. The new clinic counted ALL of my time in treatment, ALL of my clean drug screens, and gave me credit. Therefore in conclusion, all clinics are different. Some are horrible, some are alright. Not to mention There will always be that stigma that comes along with clinics. It’s the best thing that has worked for me. Sometimes you just have to do a little searching to find the right place for you.
Ur story sounds like u leave around knoxville tn. & u went 2 DR woland. 4 pain meds. & DRD 4 done ur story sounds just like mine. Except the baby. I hope u & baby are doing great. best wises Thomas Powell tn
DRD is a nightmare clinic & is run like a concentration camp, imho! Went there over a decade ago and tapered. When I tried to go back they wouldn’t take me due to a benzo script. My only alternative was to go to a clinic in North Georgia. Driving 250 miles round trip abt killed me when going daily, but now I go once every 2 weeks & feel that the situation isn’t perfect or ideal, it’s not anywhere as bad as DRD/BHG Knoxville!!!!
Hi my name is Kevin I’m from Nashua New Hampshire as I’m speaking to you I’m laying down on my futon my my right hip is totally trashed I need a totally hip replacement and the effects from my waist down my groin my left hip so much pain so much discomfort can’t sleep can barely walk can’t put my socks on and I can’t find any pain relief so I turned the street drugs now I’m addicted to heroin and Suboxone does not work for me and my insurance will not cover methadone clinics I would like to find a doctor that will prescribe me methadone to ease the pain of my right hip and get off the heroin before the heroin kills me please somehow getting back in touch with me leaving name and number and address somewhere close to Nashua New Hampshire thank you very much and God bless
Jesus Kevin. I’m so sorry to hear this. I hope you’re able to find help. I lost my brother to heroin and it’s trashed our family. My prayers are with you.
Hope you were able to get some help. I was at a clinic and paying when I was put on disability thus being able to cover my methadone. I had to switch to different clinic and put up with a massive amount of crap from a staff that always thinks and expects the worst from people. Assuming you haven’t found a place I would just start calling clinics. Generally, there is always one clinic in a large city that has state sponsored spots for low income patients and these also take medicaid. Good luck!
Look into methadone clinics call and see if they have a grant program u can go on that’s how i pay for mine.
Dr Octavian austricu west Babylon ny
However if u find another, please let me know… bc he cut me off for being positive for cocaine one time…once.. And dr safino at the hauppaugue methadone clinic would not accept me saying my issues are more pain management, even after calling oasis to fight the decision. well
I have bilateral hip dysplasia. Just had a fasciotomy for rhabdomylosis on this past Father’s Day…and so I do understand your situation CB I’m in the same boat.
Each clinic gets funds from the government called SAP funding, substance abuse prevention funding to pay for those who cant afford to pay for their medicine.
If you have the money to buy Methadone, go pay the Methadone clinic which I’m sure will be cheaper
Hi there mate. My name is Debbie and I’m on the methadone it is a life saver. Please do your best to get on the methadone ask a doctor and that should be able to get u started. Life is to short to waste. Hope it all works out for you..And by the way I’ve been on heroin before for at lest 10years and now there’s nothing I hate more then the shit and all the fucken around to get it but do your best to get on the methadone ask a doctor hopefully all works out for you. Debbie in Australia xx
I don’y know of any laws or regulations that limit tramadol to a seven days supply. It;s either a pharmacy policy or insurance company policy.
Tramadol will ruin your teeth!! Be very careful. Google tramadol and teeth. My sister had3 teeth snap off at the gum line before I researched her meds and found the cause.
Kevin, get on Medicaid! Claim independent. You will get approved in your condition. Medicaid pays every dime of my methadone treatment at our local methadone clinic whereas I would have been out of pocket $436/monthly had I not gotten on Medicaid after the first month the lady told me to get on Medicaid! Praying for you! I know your pain. I’m in Alabama BUT I do know that the !medicaid laws are mostly the same in all states.
Methadone is not what they, the medical community, thinks it is. They were apparently wrong about opioids, when in my reality, they worked great for me, now they want me to trust their new theory while treating me like crap? Methadone ain’t no better than any other opioid, except, when you crawl there every day, they have control over you. That’s what they really want, control over you. Be very very careful bud.
Your story touched me and I just had to check in to see if you have made any progress with your goal of getting on methadone? I truly hope so and that it is helping with both your addiction and your hip pain. God bless!
Any doctors in NJ that are willing to prescribe methadone ? Been in alot of accidents and been on oain meda foe years ready to stop and hopwfully find a physician willing to prescribe methadone. Thanks
This may have all been asked before but I didn’t see it. I am in Toledo, Ohio looking for a pain doctor to take me from suboxone that I went on willingly for my chronic pain to possible methadone due to the fact that the suboxone has worked wonders for my chronic pain for the last 3 years. But on top of the chronic pain I now also have trigeminal neuralgia which is horrible but doesn’t really do much for that pain. Unfortunately the suboxone blocks anything else that could possibly work for my severe facial pain. I have willingly went through any hoops an addiction doctor needed me to in order to have my pain helped. Sad that I have to lie to the insurance doc and say I am a junky to use it for off label conditions.
Go to the rainbow clinic on telegraph r in Monroe Michigan. The place is wonderful. They except most private insurance but do not except government insurance if you have no insurance or insurance they do not except it is 100$ a week. I transferred there to get on methadone program because subs did not work for me.
Dr, Until recently I was on Methadone for over 20 years for chronic back pain. Now my primary physician says my liver enzymes are all out of whack. Was wondering if you have researched long-term use on the liver if so what did you find. If you don’t have any info on this could you please point me in the right direction. Just curious!
Thank you so much
Linda
I thought i was the only one! I have to lie and say I’m am addict to be accepted at my methadone clinic. Now i have to carry that label for life. Sometimes it even makes me want to use drugs..and that’s not something I’m even into. But having to lie, go to the clinic everyday, see people’s face when i tell them what i take, all that makes me FEEL like a junkie.
Dear Dr. Fudin,I am on oxycontin for peripheral neuropathy. I am looking for a doctor in nassau county ny or nyc who will prescribe methadone for pain. for my peripheral neuropathy because the oxycontin is not helping.
Hi I was just at a new doctor in Nassau County who wants to take me off oxycodone & put me on methadone…Ive been on oxycodone for over 10 yrs & it’s the only thing that works for me with no side effects & no euphoria due to my high tolerance I guess but this doctor seems perfect for what you’re looking to do & I need a solid doctor who will continue my oxycodone immediate relief & long acting pain medication protocol
I don’t know if you will ever get this, I just saw your comment dated 2017. I’m going through the exact same thing. I’ve been on oxycode immediate reals 6 30mg a day and 2 20mg oxyneo for 11 years. I feel no high at all it just let’s me feel like a human. I’ve tried every med possible no joke and finally I can function I can actually sit and watch a full movie. I have horrible not be pain from 3 back surgeries. My doctor has decided that my meds no longer work and set up an appointment tomorrow with a methadone doctor!! I’m scared to death. I’ve tried methadone and suboxin befor and I was still in so much pain I didn’t eat to live. I wish my doctor could be in my body for 1 minute and she would understand. What has happened with you? Are you okay? I hope you are well I truly understand how u feel.
Oops typo… it should say” I have horrible nerve pain.”
If u would like to exchange info maybe we can help one another achieve our goals…I’m pretty certain I can help you find someone good for u in the long island/NYC area & hopefully u can help me find a doctor not afraid to continue my oxycode that I’ve been on for many yrs & All of a sudden my doctor got rid of all pain mgmt patients & is now doing cash only ketamine procedures…Hopefully we can help each other…All the Best
Need methadone doctors on longisland ny for pain can you help
Can someone please help me find a prescriber in the Tucson, AZ, area, who is not afraid of the new DEA crackdown on narcotic pain medication? I had a lumbar discectomy from “top to bottom” 9 years ago with the hope of relieving severe lumbar and sciatic pain on the left side. I had a competent neurosurgeon but the surgery was not successful in alleviating my chronic pain. Ever since, I have been dependent on large doses of time release morphine and for the past two years 180 mg of immediate release oxycodone to get through the day. Fortunately, I have not had to take the full 6, 30mg tablets every day, but now my PCP is cutting me off entirely. I have tried everything: many epidural injections, acupuncture, chiropractic and physical therapy. I am now considering Suboxone to relieve the dependency, but I will still be left with chronic pain. I am a 68 year old male, and hope to live at least another 10 years, but I cannot imagine doing so with the terrible low back and lower extremity pain that I continue to suffer with. Neurosurgeons at the University of Arizona and at the Mayo Clinic in Phoenix, tell me there is nothing further that can be done for me surgically. Is there anyone out there who can help? I will travel to any point in North America. Thank you and G bless all those who suffer.
Thanks for the prayers and may God share his healing light on you as well. I know the horrible ordeal you’re suffering threw and all i can say is you’re not alone and we are all in this together. May God’s love and Light shine down on us all and heal our bodies, minds and spirits! Peace be with you all!!!
If you’ve only had a discectomy, then most likely you need a Fusion. My guy did an excellent job 3 weeks ago. I had not sat is almost 3 months. I had not laid down for more than an hour. I sit when I want to now and I can sleep thru the night. SOUTHEASTERN SPINE AND BRAIN, DR. GOLDMAN!
Hey Chris,
I’ve been living with back problems since 2011. It was due to an accident on my job. I’ve had only one surgery which was called” that I fuse”. That is particularly a fusion done on my sacroiliac joint. I regret having a surgery. I have not had a day of being pain free at all. I wish I could say the same for myself as you are so happy about your surgery. I am happy for you. I wish so badly 2 get off of pain medication. I take 10 mg of oxycodone. It seems to not work anymore. I experienced so much in side effects. I look in the mirror and do not recognize myself, I actually see myself looking different each month and having new pain each month. I now have problems with both my hips. I’ve been had nerve damage chronic nerve damage in my right leg and Mild in my life. I have herniated disc and a pinched nerve in my neck, ripped in my rotator cuff as well as that bulging disc in my lower lumbar, back. I don’t know what to do, I feel so lost and also my quality of life is gone. Don’t get me wrong I have some good days but they’re so little far few and in between that it doesn’t make any sense! I also take care of for the nerve damage. One of my complaints as far as side effects with the 10 mg of oxycodone, I always have headaches migraines. I also seem to have a lot of mucus in my body. My voice is always very hoarse and raspy and I’m not sure if this is a possible side effect, but my teeth seems to be getting very weak and brittle. I’m also losing a lot of my hair. I don’t really know what’s going on and I feel like I need great advice because I am lost right now. I also like to know if anyone knows anything about having that I fuse surgery. That is a fusion of the sacroiliac joint, is there such a thing of that being able to be reversed?
Thank you for allowing me to write this in hopefully you are still in a great place in life. Wish that could be me one day
Chronic opiate use in males may lower your testosterone
I been living with chronic back pain since 2008, I got hurt working inside a prison nd I never seen a dime..I hve a degenerative disc disease, herniated disc, nd bulging disc in L4 nd L5 .I hve joint infusion in both knees, Right hip was messed up in a car accident.Im taking test now for my hip..Pain, Pain, nd more Pain…Im having a problem with mucus nd my voice since being on the Percocets.Im not a smoker .The mucus never goes away.What do you do for the mucus????God, bless everyone!!
I live n Apache Junction & can give u a Dr down here n the valley that u can drive to once a month. Try Dr Narwani. He is pain management board certified & falls n2 Gov Dukie’s new BS rules.
Good Luck
Try DR CHO in Los Alamos Vasquez. Don’t say I sent you lol?
Dr. Cosgrove at Pain South. Located in POB 2 St.Vincents Hospital, Bham, Al.
Try the sun clinic in tucson its off speedway abd jones blvd the people are great well most of them are and they have no cap so thry will take u as high as u need to go until u get relief im sure t they gab ca cut off at some point but i do know some people are on 160 mg.
Hi, did you find a competant pain doctor in Arizons?
OxyContin won’t help neuropathy. Try neurotin or similar drug
Lyrica helps better than neurotin or Horizant for me!
I live in Portland Oregon and I started taking pain meds in 01… I was in a horrific car accident and we taken on a ride of B.S. I found out I had 5 herniated disks crushed vertebrae nerve damage and a TBI…. I was put on methadone about 8 yrs ago and ever since it’s hell…. I can’t find a Dr. To help me to save my life… now all I get are doctors trying to take me off… not caring that I’m the only one supporting my kids and working on my feet all day…I’m just a number and they gave taken me from 60mgs of pills a day to reducing it by 10mgs a day till 20mgs them. 5 a day…. now I’m on .5 a day for 28 days them a big F.U. to me…. anyone know of any doctors that would help me out here???
Hello I live in OR too and take methadone but I have to go to Adapt and see there Dr because not even the VA will prescribe it. But it’s really easy with them. Just call and tell them your history. Good luck
Find a methadone clinic for addicts. It sux but a great many of us on pain management will b throwing n with persons that have opioid addiction disorder over the next year or 2. One of the clinics n my area here n Arizona said that 70% of their patients r from pills now instead of all street addicts. Kinda shocking! Methadone withdrawals after being high dose dependent for over 20 years can kill. I’m not looking forward to my future anymore…
I need help live in Salem new Hampshire waiting for surgery on herniated disc c5c6 have degenerative disc disease degenerative bone disease have 5 bulging discs all different stages have arthritis allover spine and large bone spur in spinal canal and I have garbage ins medicaid I can’t get any dr who prescribes methadone to see me I’m to poor so don’t qualify for help from obomacare they only help those that have money any suggestions on how or who can get me dr to help me I’m at the point I have to think of a reason not to blow my head off every morning thanx all you rich scumbag politicians and your theivesyou make laws and rules to make them richer while the rest of us suffer you scumb well if there’s anyone who can help me please please please help me and all you bum politicians start paying DrS and nurses and all health care workers because doctors and nurses save lives and you politicians destroy lives steal from social security so older people who unlike you worked their whole lives can’t afford food medicine or a decent place to live god bless all of you who need help like I do and bless all you drs nurses and hlth care workers who try to help us thank youthank you thank you you are appreciated
Hello, I read your post and wanted to offer my opinion on a opiate pump implant. I was in your exact position. Bed ridden 23 hrs per day and in constant pain. I don’t have a stroke thank god but I have many of your problems; like Barrett’s esophagus, hiatal hernia, gastric ulceration etc… but mostly I suffered/suffer from chronic low back and neck pain for which I just had a successful cervical spine fusion getting rid of much of my neck and arms problems and am scheduled to have a triple fusion in my lower back this coming march 15 2017. What really changed my life before the surgery was the pain pump. It eliminated 90% to 99% of my pain all over. The amazing thing is that it’s just a tiny amount of opiates being dropped directly onto your spinal cord nerves which deadens the pain very well. After a year or so after my lower back surgerysurgery I will try to reduce the dose of medication in the pump and see if I still need it. But even if I do I’ve had it for 15years now and have had it replaced three times the last just two weeks ago. It’s a life savor. I hope you can get to read this reply and that you opt to give it a try. Good luck to you.
II have both back and neck problems and had L ry2,3, and 4 fused last year and C 4,5,6 to C7 removed and total cervical spine reconstruction this past May 2017. I’m on both oxycodone and Oxycontin which helps. I am considering a pain pump implant for some time now but was wondering if it is effective for both back and neck? What type surgeon does this?
http://www.jenniferschneider.com/, Thank you for such a good article. I have been on Methadone for chronic pain since 2005. I have my relationship with my pain MD end due to his retirement in May 2016. Since then I have been looking for a MD in Denver-Aurora, CO area to continue pain management with methadone. Any suggestions? I got insurance with Kaiser and still now in Nov 2016, have not found a MD you will help me with Methadone. I have all my medical records showing proof. I am with a M D that has me on Morphine Sulfate, but it seems to be leaching my energy, which I did not experience with Methadone. Again looking for a MD in Denver-Aurora CO area to prescribe Methadone????Please help…
Dr. Roth Lawrence Kaiser in englewood
Dear Joni Naylor,
I went through a similar experience to you. The Dr. Prescribing my Methadone retired and he is the ONLY Dr. who I have found that actually understood the rug completely. He was originally a G.P. and then worked at a Methadone Maintenance Clinic for 15+ years. He understood that Methadone is one of the most difficult drugs to prescribe correctly. I am a fail pharmacy major who turned to Chemistry instead so I understand the Science very well. Methadone is a broad spectrum pain med. It also has the largest difference between individuals as far s how fast it is metabolized is concerned. Regular Peak and trough tests must be performed and then when the dr. knows your rate of metabolism a peak and trough test should be done at least once a year. Also QT wave (12 point EKG) baseline and then every 4 month retest must be performed. Methadone can extend your QT wave and cause heart problems. This happens much more often in the addiction patients than in pain patients due to the fact that many addicts have had multiple heart valve infections due to unsterile injection practices. I never had a problem in the almost 20 years I have been on the drug. I was at a high of 270 MG/day and then I asked for a reduction due to side effects and went down to 150 mg/day for about 8 years or so. I have been on a taper for 2+ years. The bad knee and back for which it was originally prescribed is being replaced in November 2017 and The CDC came out with their witch hunt recommendations for pain meds recently, in the past 2 years. Because Methadone has such a variance between individuals and a high opioid site affinity it is sorely misunderstood. I generally is not a strong as Doctors are told. The conversion charts are outrageous, and practically worthless. I don’t know what your pain is caused by soI cannot make any recommendations as to effective replacements. Suffice it to say you are in for the fight of your life to receive adequate pain management if you don’t have end stage cancer. This is the first time for me on this site and i probably won’t be back. One problem with Morphine is it can have metabolites build up that are unsafe, there is no dose ceiling or bad metabolites with Methadone. Try a Pain Treatment Center, the CDC has recommended a 100 Mg/day limit for Methadone, but Dr’s. can exceed this. There is only one Federal Law limiting Methadone and that is for Addiction Centers and is 275 Mg/day. That is a very large amount for almost any type of pain. A blocking dose of Methadone for addiction purposes varies by patients weight. It is generally on the 100 mg/day range. That will block most other opiates/opioids. Stay away from Buprenorphine, it will push Methadone off the pain receptors and cause withdrawal, it does kill pain but only about 35% of the receptors are activated that kill pain as opposed to 100% for Methadone/Morphine Etc. Methadone takes a very long time to get off of. There is only one effective drug for breakthrough pain when on a high dose of methadone, it is a relative of Fentanyl. That is another problem with it. I do not know Colorado’s laws. You may have to Doctor shop to find a willing knowledgeable one. You cannot go to an addiction clinic to get your Methadone unless you are an addict and can prove use of other opiates addictively. If they accept you for pain control they could lose their licence. I see you post is almost a year old. I hope you have had some luck and i hope this clears up some questions about Methadone for pain for others. Namaste, B.F.B.Jr.
Methadone is extremely useful in the elderly. It has almost none of the mood-altering effects that hydro- and oxycodone have. In my father’s last months of life, he was having extreme pain from dialysis in his fistula-side hand. This was a man with amazing pain tolerance, and when this caused him severe, unrelenting pain, there was no doubt in my mind how severe it was. (As “proof,” < 10 years before. his femur head and acetabulum were shattered. A small dose of oxycodone made him literally crazy – but acetaminophen alone was sufficient pain control.) After signing a batch of documents agreeing to the death-penalty, I finally convinced a pain-management doc to Rx methadone. It took 2 mg to < pain of the dialysis to tolerable, with no adverse mood/mental status effects. Methadone has such a stigma as the "heroine-addicts' drug," that it really took some serious work to get it Rx'ed. It is a terrific pain drug, with little psychological/mood effects. Doctors need to get over their prejudice against this very effective medication. Thanks for the article!
Thank you Doctor for your input can you recommend a Doctor for me in the Boston Mass. area
I will send you an email under separate cover.
Hello Dr.
May I start with saying what s pleasure it is to finally meet a Dr. who understands the uses of methadone and how it doesn’t give you that high but does give you the relief we need from chronic pain. I myself suffer from chronic pain in addition to prior addiction. I have had a Dr which prescribed it too me for many years, until the FDA came down on him and he cut me. He didn’t even have the courtesy to tell me in a visit, he had the PA call me and tell me over the phone, so my question is can you recommend s Dr on long island or any of the 5 bouroghs that would prescribe methadone to me, thank you in advance for your time,
Lisa, Please send me an email to Jeff@paindr.com.
Helllo Dr.
I have a super rare condition called suprascapular nerve impingement. Mine is not due to a cyst, so I am the 9th documented person out of dead & live cadavers in the whole world since 1959′ to have this. It took 21 yrs to get diagnosed & another 3 to find a surgeon. Or I thought, i spent all day Monday at the Mayo Clinic w/ 3 top surgeons. I have this but something else very rare going on. My muscles between my neck & shoulder are 100% atrophied. I also got rotator cuff bone spurs & tares & carpel tunnel surgery at the same time 10 yrs ago after needing it for 5-6 yrs. I have to go back to the Mayo Clinic & also to the Tampa Bay Rays & also the Miami Marlins teams surgeons also to get all opinions before I get the surgery I need. I am filled w/ arthritis that was wrongly diagnosed & I have fibromyalgia as well. I am 36 & disabled now. I mostly did hair & was a maid, but I did lots of manual labor work & lots of sports like volleyball, cheerleading, weight lifting, basketball & even played the violin. Lots of arms, arms, arms! ANYWAYS, so I have been on the pain meds that worked pretty well for 14 yrs & no increases in over 8 yrs. it got me through, unless I was in a flair up then steroids would help although I would be bedridden for 3-4 months ish… each time. So, my question I’m sorry… my meds have recently been decreased more then 50%. I am in so much pain I am having horrible thoughts. This is very unfortunate because I’ve been a perfect patient & w/ same Dr for over a decade & until recently I only had thoughts like this when I was going through a flair up. My pain is not controlled as of my big change whatsoever!!! So, I am thinking of trying to think about trying to go to a methadone clinic to be able to stay alive as no one I don’t think could survive living in this much pain. I was on 500 MME’s, now I’m on 200 MME’s and my Dr is saying he’s gotta get me to 90 MMEs… it’s just not gonna work. So, do u think me going on this methadone medicine would be ideal for me? I’m so scared!! Any advice or tips, I have potentially 7 surgeries all orthopedic coming up (mostly nerve releases). My rare shoulder one alone is gonna take 2-3 yrs of extensive therapy afterwards for some of my muscles to come & grow back. Im terrified of making a switch again after being on the exact same meds for about 14 yrs. I’m concerned about the stigma as well in regards to what will happen to me after surgeries each time & what it will require me getting prescribed after each one, etc…I wish I could just stay on what has got me by for all this time but the world has gone crazy! Thank u for any & all suggestions & or tips!! Thank you so much!!!!
Hello Sir/ Dr. Jeff,
I am super bummed because I just sent u a message on here & I am not seeing it in the comments. My arms are really bad, as u will read if u see it… so, I am just hoping u somehow got it!! Thank u so much!!!!
Thank you for your response. My pain management Dr. wants to switch to Methadone from Hydrocodone. U pray this is effective!
Methadone is extremely useful in the elderly. It has almost none of the mood-altering effects that hydro- and oxycodone have. In my father’s last months of life, he was having extreme pain from dialysis in his fistula-side hand. This was a man with amazing pain tolerance, and when this caused him severe, unrelenting pain, there was no doubt in my mind how severe it was. (As “proof,” < 10 years before. his femur head and acetabulum were shattered. A small dose of oxycodone made him literally crazy – but acetaminophen alone was sufficient pain control.) After signing a batch of documents agreeing to the death-penalty, I finally convince a pain-management doc to Rx methadone. It took 2 mg to < pain of the dialysis to tolerable, with no adverse mood/mental status effects. Methadone has such a stigma as the "heroine-addicts' drug," that it rally took some serious work to get it Rx'ed. It is a terrific pain drug, with little psychological/mood effects. Doctors need to get over their prejudice against this very effective medication. Thanks for the article!
Hi, I guess i am considered “eldrrly” since I will be 70 shortly. Being a teen product ftom 60’s, I feel &think much younger becuz of rock. N roll. It keeps us young listening. But 70 is senior. Anyhow I have been off and on methadone for years. It worked greay by adjusting it up and down. Didn’t need oxy’s for intermittent pain becuz never knew about that scenario. Then a pain dr i went to when VA stoppef treatment of addiction for us Vietnam Veys wr were stuck. The pain “specialist” put me on oxy with methadone. That got me into thinking I needed breakthrough meds. Now I actually do because of low dose of meth. Us Vets were on minimum of 120 mgs of meth. I knew guys on 300 mgs. Anyhow, with all the ODs blamed on methadone DEA has drs cutting way back. Problem isn’t meth its the mixing of dtugs lole xanax or to many oxys with meth but if one is used to meth its actually safe and works best for real pain.
Hi Dr. I am hoping you can reply! I am trying to find out the difference of methadone vs ‘s oxycodone. I just went to Dr and asked to go back on oxycodone. Mistake? He told me now don’t come back in a month and want to change back. You know I am not comfortable with changing like that. I have chronic pain everywhere! Now shoulder problems! A tear on shoulder. Something going on with left one too. From what I could understand. He is quick than out of the room after only one shot in one shoulder. Have to wait 2 weeks for shot in other. Anyway I am so scared I made a bad choice!mudy try n change it right away! I know Oxy comes on faster than methadone. It’s my back too! L-3 at 5mm broad-based herniated. Causing great upper front thigh pain. Already have sciatica in back of legs. Fibre as well. I am in to much pain. Should I have stayed on methadone? I am resding how hard to find Dr to prescribe methadone. I have been with my pcp long time. To nervous to change that type Dr. Am seeking out specialists for all my problems . Oh god my right shoulder hurts so bad! I know I should have break through pain meds with the methadone. I am a serious subject. With intence pain issues wanting my life back so bad! Last surgery in 2012 ruined me! He just made a mess of me! Pushing my sister in wheelchair didn’t help my shoulder matter. To take her outside while in s nursing home! Made worse when getting stuck in doorway trying to move her in chair. Already was a caregiver for elderly with dementia that hurt my back 2007.since then my life has been over. Dr’s to afraid to help me. Do I think i should have stayed on methadone? Anyway to advise? The phone number given always busy.
Kim, For long-term use, methadone is often better than oxycodone for burning/shooting pain which we call neuropathic pain. For shoulder pain oxycodone and methadone could be equally effective, but everybody is different. One thing is for certain, methadone should only be prescribe by someone who is expert in that area and has signfcant experience prescribing it.
You know I knew there were alto of people on methadone but my situation is the opposite a little, I have been on pain mess for the last 30 yrs and I been on methadone for 20 of those years well as you can guess my body is amuse to it i went to a methadone clinic in the past then I got a Dr. Which differently saved on my budget that Dr. Put me on 120 milligrams in the pill form which was 10 milligrams each . Well then of course she referred me to a pain specialist and he told me the max he could put me on is 80milligrams 1 to 2 every 4 to 6 hours. I’m sure you have figured it out for 3 years I was on 120 milligrams liquid everyday and then get dropped to only 80 milligrams. Needless to say they were helping at least 35% but now they just keep me from going though withdrawal and if anyone has ever and I mean ever went through withdrawal you know what I mean when I say it absolutely scares me to death to go in and tell my Dr. That the methadone don’t work for my pain is there anything else that he could put me on. And would not go thru withdrawal from stopping the methadone. Please if anyone out there has ANY advice please in begging you to reply to my problem. And I thank you a thousand times over for just giving me your advice on this situation.
As far as not wanting to go thru withdrawal effects… I would suggest speaking to your physician about Tramadol. It is also a good pain mgmt medication. I have read various stories how “it is weak”…”Tramadol is crap”…my response to that is, “if your just looking for to get ‘high’, then yes it is, but if your looking for pain relief & or relief from withdrawal, then this is perfect. This is coming from me, a man that was at one time on Soma 3xday, OxyContin 80mg-2xday, Methadone 10mg-4xday and Dilaudid 16mg 3xday. I was on it all at the same time, I was being overdosed by my PM doc and didn’t know it, until I was hospitalized. Only thing I ever wanted was pain relief, in order for my new Dr to provide pain relief was to take me off all the drugs and start over so to speak. We did that with Tramadol. It is also much safer than a lot of the other drugs.
I hope you find some relief, I do know what it’s like to be in your situation, I wish it on no one. I am sure you have found a solution to your issue as you posted this in Aug, but just my 2cents… Be Well-Peace be with you
Thank you for the informative and balanced article. As a chronic pain patient I can tell you that I really resisted the changing of my primary pain control drug from controlled release oxy drugs to methadone because of the stigma in my mind. My doc, who I trust with my life and is one of the finest physicians I have ever known, got another patient to speak with me about his experience switching from oxy based drugs which were ineffective even at high dosages, to methadone and he said the difference in pain control was like night and day. I metabolize oxy in a very strange way in that the analgesic metabolite, oxymorphone, does not get into the therapeutic level even at very high doses and my P.M. physician discovered this by having me take my normal dose a certain amount of time before my appointment and then got blood and urine samples from me. It revealed something very interesting. I was retaining the metabolite noroxymorphone (which to my understanding has little or no analgesic effect) and urinating out the oxymorphone (the active analgesic metabolite). This was over 5 years ago, BTW. My previous physician could not believe I was not getting satisfactory pain management on high dose oxy but was having all the nasty side effects. So, I gave methadone a try and my dose was titrated over a period of a month or so to 20 mg p.o. b.i.d. (total of 40mg a day) with very satisfactory results, and in 5-1/2 years the dose never needed to be increased. It was not elimination of pain (which I did not expect) but brought the pain to a tolerable level (multiple herniated discs with nerve root impingement, bulgers, spinal stenosis, ankylosing spondylitis, etc.) so my life did not center around waiting for the next dose of medication so my pain would be decreased. As a result, I have been able to wean from 40mg total a day to 15 and am hoping to continue to reduce until I no longer take it. I am lucky in that opiates do not give me pleasure – they give the jitters and a tightness in my neck and throat, especially oxy, so there is no psychological desire and sometimes I forget to take my PM dose. The nice thing about the long acting nature of methadone is generally one is not awakened in the middle of the night by searing gluteal and leg pain since methadone because of a skipped dose. Oxy for some reason works fine as a BTP agent but not a a primary drug. Even then it gives me an uneasy feeling, like I have stayed up all night then had 10 cups of coffee. If anything. it is displeasurable but it does take the sharp edge off BTP. i have also reduced the amount of that I take by 50% and am trying to eliminate it. Again, although my body is somewhat dependant, I am not psychologically dependant because I get no pleasure from these. The methadone is like taking ibuprofen for me – I don’t feel it at all except the analgesic effect which is much slower to “kick in” than other IR opiates and does not cause the uncomfortable stimulant effect. Thank you for a) labelling all people who take these drugs under the supervision of a properly trained pain management physician as “addicts,” (and I make no judgment about that because if it gave me intense pleasure I might be more inclined to crave it; it is a CNS condition that varies from person to person) and b) not labelling those who are on methadone maintenance for heroine addiction as defective or bad people. Your article was very fair and balanced from a patient’s perspective and we need more physicians like you writing articles like this than those who will not prescribe an opiate stronger than hydrocodone even if the patient has legitimate, severe chronic pain, villifies and labels patients as “opiate seekers” because they complain they do not get adequate pain control from hydrocodone. Each patient is unique and requires the proper combination of medications carefully titrated. It is not a one size fits all treatment and we need more compassion for those who have severe chronic pain that only respond to opiate therapy and can continue to function in their lives intead of leading lives of unmanaged pain, not addicted to medication but simply want reduction in intolerable pain. Only those who have experienced debilitating pain that does not let up can appreciate how frustrating it can be get adequate pain management without being stigmatized, given dirty looks by pharmacy employees, and spoken about behind their backs by people who have no idea what it is like to be awake for days on end in searing pain. I see a lot of comments calling anyone who is in an opiate pain management program an “addict” who make perjorative comments about people in constant pain. I hope those people never have to rely on pharmaceuticals to manage severe pain yet at the same time if they had to endure it even a month I bet many of them would change their tune. Thank you.
oops… “thank you for NOT labelling all people who take these drugs……….”
I was in boot camp at Parris Island, got strept which later caused me to be covered in psoriasis ox 90% of my body for 20yrs. Then caused psoriatic arthrits to my misery and now fibromyalgia also. Ive been on pain meds for 21yrs. Oxycontin / percocett to morphine er and msir. Because of all the bad publicity i have taken cut for last 3yrs. 690mg for 6yrs to 460 to 360 mser & msir. Now my md wants to cut me to 300 mg mser. I cant handle this cut. Ive been his pt for’15+ yrs. I have never faile a drug test in 69 test. Neuer came in early, never asked for more. But ive tried and 300 is just not doing it. I cant even think strait, my body wont work right. I take care of my mother with alzheimers/ lewy body dementia for 13yrs now. Any way im on Humira inj and at 360mg i would always tell my md that i hurt but im not in misery, so im just find with my meds. Would i be better off to ask him to change me to say 80mg methadond a day with 10-20 of msir or oxy for breakthru. Would both meds work toge her? If he added 10mg bid methadone to my 300 mser, would it help me. Wovld the methadone stop my morphine from working? I really need help for some advice. My md said if i just couldnt handle the cut from 360-300 to come back early this time. Is methadone my answer? Please help and thank you so so very much. In acute distress!! Brad from Newport
Ed, Thank you for your sharing your story in such detail!
Thank YOU and Dr. Scheider – you are both physicians who seem very patient oriented and knowledgeable. It is great to have a forum where we patients get to interface with you docs, in a positive fashion. My backrgound is molecular biology/biochem/cell biology. I am NOT a doc despite my long responses. I just want to help people who have been in the same situation if I can. Thanks again!
Been on methadone as replacement for Herion misuse for 12 years because everytime i have a drug worker and am getting places the drug worker leaves, there is a terrible turnover of workers in the drug problem centre in Dundee Scotland GB, i was on 70ml and using benzos aswell, i asked for help with benzos and after only 3 or 4 sessions with a new young worker she came back with the answer we will NOT HELP your benzo misuse but need me to come down once a week to give a urine sample as they decided i still had Herion issues, now i’m no saint but the benzo withdrawel treatment i had with the service came with no drug worker as the 10th at least worker i have had in the 12 years backed her job in so i was being withdrawed but had no worker help and as i said the new worker i have had 3/ 4 sessions with came back with the answer we will not help your benzo abuse which i am screaming for and ready for at 40 years old and now attending college to acquire Accounts Diploma Mon to Weds 1st year and they after not seeing me for 8months plus then wanted me in once a week for urine sample for herion which i have no problem with, i felt as though she was punishing me and after a heated argument i told her” yes i want off my Meth as do all the people in this service”, 1 week later 10mls was taken off my 70 then 5ml a week til 35ml which i am still on,she says this will continue for another 7 weeks then i’m off it and no other treatment afterwards is being offered am i mad or is this a very harsh treatment for which i thought was jst an argument and as i said i have been on at least 70ml to 110ml for last 12 years until 6 weeks ago i am on 35ml now and phoned my drug worker/mental health nurse and told her i had suicidle thoughts her reply ” phone your GP” IS THIS RIGHT/ OK…REPLY FROM REASONABLE DOC WOULD BE GREAT AS THIS IS IMPACTING ON ME AND MY FAMILY I EVEN TOLD THEM IS IT WHEN IM AT THE END IF A ROPE IS THAT WHEN THEY WILL TRY HELP OTHERS BETTER PLEASE DOCTERS ADVICE NEEDED?!?
iam kristie jenkins iam 46years old and sufffer chronic pain i became addicted to opiods from kidney cancer an disc deteriation sydrome also arthritis through all my joints i was kicked out of pain management because i got out of control an did not understand what was happening in my brain . iam now taking suboxone which is not controling my pain do you have any advice where i could get help for pain the suboxone does not control my pain an i was on morphine an methadone for 7 years at the james pain an palliative care at osu hospital please help
Thank you SO much for your insightful thoughts and personal experience with methadone and other opiods as tx for chronic pain. I, too, had an awful time with getting adequate pain reduction and, after chewing it over, decided to try methadone. I was nervous because the dose seemed awful low compared to the multiple daily doses of other opioids. When I was on the methadone, however, just a very small amount was significantly helping my excruciating nerve pain from Type 2 Diabetes. We had to titrate upwards only a little bit, but I love that it does NOT give me the euphoric and drowsy effects AT ALL!! It may be nice for some people to feel euphoria but I like to feel balanced and like myself, if possible, at all times. Anyway, after understanding conversion charts, I was more than willing to take this journey as literally NOTHING WAS EVEN coming close to relieving my nerve pain. Nothing… no matter the dosage!! So, I am so very grateful for meeting a doc who is familiar with using methadone for chronic pain and I was willing to be my own advocate, study and research for my own safety, and take methadone as prescribed. BTW… I so wish more people would educate themselves about what’s out there to help others AND help themselves. What’s good for the goose isn’t always good for the gander and stigmas and fears can be erased with education. Thanks again, Ed and this article was wonderful as in it was fair, with its good/bad sides to choosing methadone for tx and choosing to prescribe it for chronic pain.
Hey, just wanted to compliment ur post Brother. I am very glad u found methadone but am very sorry & sympathetic for ur life of pain.My husband & I have helped many pain sufferers find better quality of life by switching to methadone over the years. The oxy’s seem to have a roller coaster effect but methadone is very stabilizing.
Good luck & G.B.
Can you see a pain specialist if your on suboxone? From what I’ve been told is there isn’t many opioids that can break thru the suboxone, so my thought is you wouldn’t see someone that’s on it, unless you would switch them over to methadone. I’ve been in chronic pain for years, but terrified, terrified of methadone, but the more info I’ve been reading, may not be a bad choice for my pain. I’m so sick of being in pain 24/7 but pretending to everyone that I’m ok. I did have a problem years ago with opioids, that’s why I went on suboxone, and since I’ve been on it, opioids are the last thing I think of, sure when I had issues, it was on my mind 24/7, but I wasn’t using it for pain. I don’t have any kind of life. I’m in the house all day, every day. I’m depressed, anxious, sad. There isn’t any hope, no future, just pain. I don’t like to complain about it, but if there was hope to get my life back, I would be thrilled. Also due to my chronic pain, my kids haven’t suffered, and I feel terrible, but my walking is extremely limited, I had my 2nd anterior/poster spinal fusion June 2015, surgeon As great, but I’m still in the same amount as pain pre surgical, therefore I wish I never had this last one. And I’m supposed to have surgery on my neck at some point. What’s the point? I don’t think I can deal with anymore pain. If you think you could help me, I would be forever grateful. Thank you.
Dee, I “feel your pain.” Before methadone, which I REALLY resisted, even at high dose oxy I was in constant moderate to severe pain. Once my methadone dose was properly titrated it was like a window had been opened and the pain rushed out. I still had pain but it was tolerable. For me methadone also is a lot more “even” due to its long half-life. WIth oxy 1-1/2 hours after I’d take a dose the analgesic effects would start wearing off (it took 45 minutes to take effect, so I had about half an hour of tolerable pain), whereas with methadone I can easily go 8-12 hours between doses (some people need smaller quantities closer together but for me twice a day is fine). Plus, I don’t get the uneasy, jittery neck and throat tightening that oxy products give me. Each person is different but if you are inclined and your physician thinks it is appropriate I’d recommend at least trying it because it truly changed my life from one centered around pain to one where pain and its mitigation were not the primary focus of my existence. Good luck to you.
Hi Dee, hopefully by now you have found an answer. If not, when my doctor suggested Methadone I was like “no way:” he told me that it is the newest answer to pain without the addiction, euphoria or sedation of other pain meds. So I went on a low dose and it was like a miracle. I have Tarlov tumors inside my sacral spinal canal and was literally bedridden for a few years. After starting the Methadone I still had pain but it was so much better, I can’t even tell you the difference. Since then have found a neurosurgeon at Stanford hospital who takes medi/medi and he incised the tumors inside the spinal canal and it took pain completely away for five years. When pain came back as the tumors returned I had to restart the methadone and it has saved my life and sanity. Will be back at Stanford soon but wanted you to know it is not anylonger the stigma attached to it as being for heroin addicts. It is a great medicine for those of us who suffer from pain and want to still function and feel normal. Best of luck and do hope if you have not yet be open minded about methadone. Good luck and blessings to you.
Maryann Hunter,
I know response is wayy past the original post, and therefore the odds of you seeing this are slim. But my emotional response to reading your “story in a nutshell” just hit me with shocking similarities. I felt like you described my current life, while at its all time worse. Amazing the descriptions you used. I can now only HOPE i also am able to get rather better, thanks to new and better caring doctors overall. But while in such deep depression and daily severe pain, when the days/months/& now years are flying by while you cant/dont shower or dress or drive or leave home etc…..how do you suck up enough energy to fight for yourself and start making the proper calls and attending appts etc?? It all seems soooo overwhelming as of now. Impossible rather. As if ive given up. Dont know where to start nor hav the energy. But oherwise, i truly feel i, just waiting to die. I just ONE doctor out there would listen to my many TRUTHFUL physical complaints and worries and questions. I sure wish there was a way i could talk to you petsonally Ms. Hunter. In case you randomly do see this one day, please know your post was a true inspiration to ME (at 3:30am while randomly finding this page after googling appropriate methadone doses, due to my own concerns…which i find sad that iii as the patient has to be the smart or cautious one researching what my doctor is telling me to put in my body, even tho i kno my body and mention that i dont think its right, or the methadone amts plus the cocktail mixtures of pills. Smh)
Anyway, hope youre doing well. Thanks for sharing and helping another soul,, who knows exactly word for word what houve gone through. Glad to kno im not crazy or alone.
Oh and again, anny advice on how to gain the strength and hope to finally make the first step to attempt to get your life back?? (after realizing not Alllllll drs are perfect or genuises or have patints best interests in mind or how many cant admit theyyyy may be wrong and a patient might know whats best for them better than their own ego)
Peace, love and Respect,
Kerryann
Apologies. I Meant this post to be a Response to MARYANN HUNTER below
Kerryann…please contact me..I never saw this site before and I understand how u feel! You’re NOT alone.Please get in touch
Thank you
Hello,
I am a part of a methadone clinic and am on 140mg daily, and am going to be increasing my dose once my EKG results are in. Once I hit 120mg my doctor ordered an EKG qtc Interval. My question is, if they find something wrong with the results, is the standard procedure to reduce the patients daily dosage? And how common are these problems with patients on higher doses of methadone? Thank you for your time!
While not rare they are also not a large percentage of patients. The problem is this kind of arrhythmia or lengthening of the Q-T interval of the cycle of conduction in the heart can be fatal, as can respiratory suppression. That is why physicians start at low doses and gradually increase them and take EKG’s for conduction issues secondary to methadone administration in some patients.
Hello Callious,
I know exactly what you are going through. I’ve been on methadone for 10 years, been stable, and I was able to function normally. All of the pain hasn’t just disappeared, but I was able to work and SLEEP. The place I work at, changed their policy and do random P test, and if you fail, you are fired. This doesn’t apply to everyone, only people in maintenance and security.I went to a lawyer, and was told i couldn’t do anything until i was fired.. Meanwhile I got off of methadone,which was terrible. I couldn’t sleep, was in great pain. My doctor tried to help with Rx motrin, but as you probably know, it doesn’t help at all. So I finally got a steroid shot in my spine, which was great for 2 months. Now I am back to square 1.. I was referred to a surgeon who said an operation might work, or not.
i cannot see how companies can do this, when i am under doctor’s care and have been working there for over 10 years without any problems.
They give this to cancer patients, so those people have to quit their jobs and just die???
I was wondering if you had any progress in this matter, or how you are handling this.
Thanks
John, you may want to consider discussing this with a disability attorney. If it can be demonstrated that you are mechanically and/or psychologically disabled by chronic severe pain which requires supervised pain management you may be able to sue the company for violation of the ADA. If this injury occurred while on the job or as a result of the job, the employer may be liable not only for your compensation but for continued therapy and pain and suffering. I do not believe in frivolous litigation but am an employer myself who has had employees that took varous medications and our policy was specific that the ONLY time taking a prescription drug could be grounds for dismissal was if the employee was not prescibed the drug or was taking it in an other than prescribed fashion. I am not a lawyer, but that is a tact I would try. Plus, any responsible pain management physician does urine testing to make sure the patient is not taking non-prescribed controlled substances and IS taking the medication prescribed (as opposed to getting it and selling it, which some people do). Have you asked your physician to write a letter that you have chronic unmanageable pain which requires a certain controlled substance and that your employer should contact him/her with your permission (you’d have to sign a release for your company to get the information) in writing? The letter must be very specific and admonish your employer that such information is confidential medical information and per federal statute your employer is required to employ control measures to keep that information confidential and with limited access ONLY to those you authorize to see it, in writing. Refer to the federal HIPAA statute. If you are certified as having a disability your employer cannot really even ask you anything more than that, i.e. what the nature of the disability is, what medical treatment you receive, so long as you are able to perform the duties of your position and did not misrepresent yourself at time of hire, e.g. by claiming you could lift 50# sacks of concrete if the job required lifting 50# sacks of concrete, and you could not. Companies large and small have to comply with federal statutes such as the A.D.A. I’d try the physician letter route first and if that did not work file a suit (if legally advisable) for the reasons above, or whatever your attorney deems appropriate. If you carry a sidearm, baton or other enforcement device the company might be afraid of the liability should someone be harmed by an employee who is taking an opiate such as methadone, or fear a possible suit from another employee who takes methadone for recreational purposes who is dismissed on that basis but not for dissatisfactory performance. The problem is most people do not understand that when titrated and taken properly, it is not a drug that automatically makes you “stoned.” They seem to have this vision of people who take methadone as a bunch of derelicts laying arund in a crack house, high as kites. While this may be possible for some a responsible physician will not over prescribe and will monitor your compliance with testing for both her/his and your protection. The fact that you would rather work than lie around with disabling pain might be a good point to raise if the matter unfortunately requires litigation. Sometimes company policies are in violation of statute and in that case are unenforcable and grounds for challenge in court, with coimpensatory damages as well as getting your job back or an agreed upon financial settlement. Hope that helps.
Just a fyi methadone tests are more expensive so i highly doubt the testing of methadone would be included in a employment drug test. I’m a truck driver and Dot doesnt even test for methadone so chances are if you said nothing and took the test you would have passed because it’s atleast over a hundred dollars to test for methadone because it’s a synthetic so it doesn’t show up like your regular opiates
If a drug is prescribed the urine test company reports a clean urine to your employer…they are not allowed to discuss controlled substances that are under valid prescription only illict and non prescribed drugs…you went through all that for nothing when a simple letter from the prescribed physician is all you woulda needed
I’m a methadone patient and have been on it for nine years. I am bi polar and have been an addict to pain meds for many years due to spinal disease. Now I have stage four colorectal cancer metastasized to my liver. After a colon resection and chemo and losing more than half of my liver, I am inrremission. My question is this, should I use only methadone for pain sixty mgs daily is my dose and use ten mgs roxicodone for breakthrough pain, or just use methadone alone. I have been told that mymmethadone is probably blocking the roxicodone. I am worried about the effects on my liver as Ijjust had surgery four months ago. I also want to protect my liver. Thank you.
Erica,
Methadone does not block oxycodone, In fact the two of them have more combined opioid activity. Whoever told you that methadone can block oxycodone is probably confusing it with buprenorphine.
I really need your advise about my current situation. Just to bring you up to date, I am a 45 yo female with chronic back pain (herniated discs with nerve impingment) and DDD. I live in West Virginia and have been a patient at a pain clinic for a year and 9 months, my former doctor retired. I have been on Methadone for 12 years, it is the only medicine that helps my pain and allows me to lead a productive life with back pain. When I came to this pain clinic, I was taking Methadone 30mg TID. The doctors there have told me that I am on a terribly high dose and have taken me down from 90mg/day to 60mg/day in just 4 months. I asked them why they were cutting my dose and they said that Methadone is a “dangerous
medicine” and that I needed to be taken off of it. When they cut me down, they prescribed me Oxycodone 15mg QID to take along with the Methadone 60mg a day. But the oxycodone doesnt help my pain, ive had other doctors that have tried to put me on it before and it does nothing for the pain.
I would be willing to stay at the 60mg a day dose if they would just leave it alone and stop cutting it. They keep saying that the federal guidelines say that the dosage is too high and that it could cause me to overdose. I am and have been a responsible pain patient. I even had my labs drawn and an EKG done and brought them the results, to show that everything was okay and that I didnt have any Q-T wave problems. I dont know what to do. If they take me off of the only medicine that helps me, my life will fall apart. I am a nurse, I work, I have twin teenage boys, I am a productive member of society. I have tried to find a doctor that knows about Methadone in WV but am having trouble even finding a name. The doctors that I see now are not that familiar with methadone and act as if they are afraid of it. Can you please tell me if 60mg a day is considered a high dose for chronic pain? And if there are any federal guidelines in WV that say I cannot have that dosage? One last thing, do you know anyone in WV that specializes in chronic pain management that would prescribe Methadone? Thanks so much!!
I have had a similar/but different situation, I have been on methadone for 10 years until recently my job said I couldn’t take it anymore. For the 3 months I was off the methadone my life was miserable. I went back to work but then they pulled me out again when I asked about switching back. I really don’t understand their logic. If a medication works, shouldn’t that be the one used? I’ve never heard of anyone braking into pharmacies for methadone but the OxyContin they were more than happy to hand out and let me work while taking. Hope you’ve found a doc that has helped you. I have to work through a lawyer, and doctors and lawyer are like oil and water.
I am not a doctor but was a scientist and am more educated than the average Joe about opiate analgesics.. Appropriate dose depends on your weight, “surface area,” blood level, and importantly, how effective is it in controlling your pain. My understanding is that 90 mg/day is “moderate dosagel” and “high dose” kicks in at 200 or 300 mg or more a day. If you only weigh 100 pounds that can be very different than someone who weighs 200 pounds. If it takes your pain away 100% some P.M. docs consider that over-prescribing and would rather back off and Rx a little less methadone with a secondary med such as oxycodone for BTP. If you feel NO pain they can’t tell if you are getting the right dose or more than the right dose. Erring on the side of “too little” is much safer than “too much” because opiates are respiratory suppressors and I’d imagine you’ve read the horror stories about drugs like fentanyl, which is prescribed in MICROgrams, not milligrams, usually delivered by a skin patch.
Methadone does not generally require the constant increases that oxycodone based drugs do to achieve the same level of analgesia over time. Has the clinic suggested controlled release morphine sulfate drugs such as Kadian or MSContin , buprenorphine (Subutex, Butrans, etc.) or Opana ER (oxymorphone)? If your body does not efficiently metabolizxe oxycodone into oxymorphone, prescribing straight oxymorphone sometimes works where oxycodone did not. Oxycodone does not work for me either as a primary pain control agent but works great for BTP with methadone for the primary drug. The problem with buprenorphine after methadone is you have to get your methadone levels WAY down and actually deal with increased pain and getting into a withdrawal state before transitioning to it. Patients give mixed reviews about its effectiveness. If you are taking other drugs that use certain liver enzyme pathways (like the cytochrome P450 pathway) it can decrease the effectiveness of opiate anelgesic drugs not to mention tax your liver, As far as oxycodone as as an opiate analgesic, since it is ineffective for you the clinic should know to get simultaneous blood and urine samples from you and look at the various active and inactive metabolites of oxy (oxymorphone and noroxymorphone) and see if the ratios in your blood and urine are in the normal range. I am a “reverse metabolizer” and pee out the analgesic metabolite oxymorphone but retain the inactive or minimally active metabolite noroxymorphone, because noroxymorphone does not cross the blood brain barrier easily if at all.
Some pharmacies are now requiring a “letter of medical necessity” from your doctor as CVS does in some of its stores (if not all of them). Some pharmacies claim they have no control over how much opiate analgesic inventory they will get each week (my local Walgreen’s) and that they are frequently audited by the DEA. Some pharmacies are not even willing to add new patients who are prescribed opiate analgesics. My PM doc has a contract with each of her patients and it names the single source pharmacy where the prescriptions will be filled (the patient’s choice) and only if that pharmacy is “out” can a patient get it filled elsewhere and has to give her office notice of an occasional alternate pharmacy.
Given your history it is surprising the prescriber does not perform periodic liver function tests, chemistry and hematology panels (including clotting factors), urine drug tests and EKG’s. My PM doc does all these things. She is on the faculty of an internationally known, highly regarded medical school and hospital and sits on various legislative advisory committees and has told me the DEA is making it a nightmare for prescribers. Here they are fingerprinted, like criminals. Unfortunately this translates into difficulty for the patient and liability for the physician.
There are many peer reviewed papers in medical journals that deal with methadone as an effective pain management drug and you might want to just download these and casually give them to a physician who is not comfortable prescribing methadone since you have taken it for 12 years with good results. Don’t come on too strong – docs have spent often more than a dozen years in training and don’t like to be told how to practice medicine by someone with little or no medical or scientific education. If the physician/clinic managing your pain in not familiar with methadone as a primary opiate analgesic, and does not perform routine blood and urine tests and an annual EKG, I would question the competency of such a prescriber of opiates for anything other than emergency use. I have no problem with physician’s assistants but some clinics will use them to prescribe pain management drugs under a supervising physician’s license. For a trip to the ED/ER for a badly sprained ankle, or broken bone I’d have no problem with them prescribing a week’s worth of pain medication. When it comes to a patient who has a complex medical history on long term pain management I would avoid such a practice because the education in pharmacology, neuropharmacology, biochemistry, neuroanatomy and physiology, hematology, and many other advanced courses of study in undergraduate, graduate and medical school for years to become an MD are not required to become a P.A.. I wouldn’t feel comfortable with someone who knows less about opiate analgesics than I do to prescribe my medication. A P.A. may only have 18 months training at a community college. The doc who wrote this article seems very knowledgeable and competent and I would go to see him if he was in my area if my doc retired. See if there is a faculty member of the University of W.V. medical school that has a private pain management practice. Have you considered seeing a neurosurgeon for pain management or pain management recommendations? What about contacting surgery centers or anesthesiologists, since some transition in to PM? Sorry for such a long response but I wanted to give you my take since I have had the same issue with oxy as you and have PM physician I would not trade for anything. She is tough but fair and will not let me suffer excessively.
Are you still around here? Would it be possible to have a private discussion regarding methadone benefit/risk and maybe a third person perspective since you seem to be intelligent and well informed? I have a relationship with someone in a similar situation and I’m at odds with the whole ordeal.
I just have a simple question, and am hoping to find an honest medical professional to answer me. I’m 51 yrs. old, and at the age of 45 I needed to see a pain mgt. dr. for chronic coccyx (tailbone) pain. They referred me to a surgeon who wanted to replace 2 discs, however..i repeatedly told them that, though I had pain in that area, it was not the unbearable pain area that I was having. (I also told them that i had seen a chiropractor who took x-rays, and said that i had a broken tailbone that must have gone undiagnosed) Since I opted ‘not’ to have unnecessary surgery, the pain mgt. dr. tried to control my pain with methadone and dilaudid. They also did a disc-o-gram, and decided to try spinal injections where “they” thought my pain was, instead of where “I” said it was) As months went by, I complained of swelling (enormous!!) in my legs and feet as well as my hands and upper lip closing up on their own. I had only seen the actual dr. twice, ever..over the 5 years I worked with them..Nurse practitioners were the ones who prescribed and changed my meds. From dilaudid, to morphine, to percocet, to fentynol (and probably about 4 more changes, but cannot remember the names of the prescriptions) and also adding in drugs for seizures..and refusing to take me off the methadone that “I” felt was causing more health issues for me. At one point, I woke up in the middle of the night with the sharpest pain in my right arm..it literally lasted for 10 hours, easing up on about the 11th hour. It began about 1:30am and by noon that day the pain was almost gone, but my right hand had “closed up”, as if a crippled persons hand would be. When i mentioned it to the np. her suggestion was that it was “not” a heart attack or stroke, but she knew of a patient that had slept on her arm wrong, and it took several weeks for her arm to get better. Though I swore this was not the case, I “only” sleep flat on my back with my lower legs elevated with pillows…She then suggested I see a neurologist.
I saw a neurologist, who did a nerve conduction study on my right arm and hand. Results were fine, so she suggested that it was mental stress and recommended a psychiatrist. (what a joke, right?) Needless to say, I know my own mind, and am a very spiritual person..making my life quite happy with my children and grandchildren, counting my blessings every day…I knew this was physical, not mental.
Every month I had left over medicines..as I ‘only’ took the break thru meds. as needed. Some months i could schedule my appointments for 5-6 weeks instead of 4. At one point, I had an absessed tooth over a holiday weekend. I had been on these medicines long enough that I had built up a resistance to the med. I was on..I knew I needed an antibiotic, but couldn’t get in until the upcoming Tuesday to see a dentist..so I did what I “hoped” would help, which was swish with warm salt water and stopped taking the percocet, and switched myself back to the left-over morphine I had in a cabinet from months earlier. The following Thursday, I had an appointment with pain mgt, and they gave me a urine test. They filled my prescriptions, and I had even showed her that my dentist added Tylenol 3 and an antibiotic to my medicines. The following week, I received a letter in the mail stating that they were refusing me as a patient as they felt I was using street drugs!! They said my test showed more morphine than percocet…and yes, I ‘do’ understand now that i shouldn’t have changed the meds myself..but, they did it every couple months, and I honestly felt they knew I never used a full months supply anyway..Nonetheless..That was the very best thing that could have happened..
I found an Md. who, I explained this entire story to. She was almost furious at how “over medicated” they had me, and she immediately sent me on a series of tests. She did an ekg in her office, and ordered a T-test, referred me to a ‘good’ neurologist, cardiologist, sent me for breathing tests, and a GERD dr. She did gallbladder tests, liver, everything from head to toe. I had been nearly bed ridden with illness for over a year, and pain management complained about 3 days of me switching my meds..Turns out, I had a hyated esophogus, gallstones, several silent strokes, clogged aorta, clogged arteries in the brain, and copd..ulcers in stomach and esophogus, She immediately filled my prescriptions, and it literally took her months to receive my records from the pain management facility. (and i didn’t even mention that, on my way down the hall way at pain mgt, the nurse practitioner tucked her head inside the “dr.s” office to tell him the neurologists reccomendation, ( to see psychiatrist), and how unprofessional they were to laugh hysterically in front of me…I was looking for an answer as to why i couldn’t put deoderant on under my left arm, couldn’t cut my own meat, couldn’t “open” my hand!)
It has taken 2 years to ween down, as they had me wayyy over medicated, and I’m excited to say that I am OFF methadone, weened down from 100 mcg fentynol to 25! and only taking 7.5 hydrocodone 4 times a day…BUT, also on 2 inhalers, aspirin for stroke, and 2 prescriptions for ulcers and acid reflux.
My question is, are pain management dr.s required to give regular ekg’s to patients on methadone or any of these other medications? I have been very very sick, trips to the er thinking i wouldn’t make it another day at times, and at last found a great group of doctors working together to get me back to as good of heath as possible. I’m still in bed 23 hours a day, as I think the fentynol is making me soo hot, every movement makes me boil from inside out..I’m under a ceiling fan at all times, and since i’ve been laying down for so long, every muscle i “use to” have is gone. I went from working 50-70 hours a week for Aldi grocery stores, to having the strength of a 70 yr old woman. I barely make it to the elevators with a cane, and have to sit. I was NOT this ill when i began seeing that facility, and I just want to know if they were careless with my health? Please, the pain mgt office I go to now, his np told me that methadone patients should have ekg’s every 6 months, but i didn’t know if that’s just how he runs ‘his’ office, or, if that is fact..I was too drugged before to realize that, I’ve been missing out on my grandsons’ baseball games, my granddaughter’s orchestra performances, I can’t even do my own shopping..my daughter does it for me on her day off…I get out once a month or so when i have to force myself to go to my dr. appts, …other than that, it’s not worth it to force myself to be up and about long enough to shower and dress..my life, as it was, is over. The life i have now, is waiting for my children to have enough time off work, practices, and their own chores, to make it out here to visit with me. I ‘do’, now, suffer from depression and anxiety.
Last, but not least, my new pain mgt dr. sees me each and every month, has gone through a series of spinal blocks to the coccyx nerves (which didn’t work), and showed me on the monitor where, my tailbone was indeed fractured…in several places. We are now on my 2nd trial for a neuro stimulator, as I hate, and always have hated..taking medicines..The first one did not work well for me, so they are going to place this one upside down. If it doesn’t work, my last resort seems to be a pain pack implant…which I really don’t want, but may not have a choice. Living with pain each and every minute of each and every day is exhausting, and gets my full attention. Living with the pain and nausia and stomach pain from not eating when my back pain is too much for me to get to the kitchen to get something to eat, enhances it by 5, laying on my back with a pillow over my abdomen, and knees drawn as high as possible due to pain on both sides..is just too much, but even worse is the loss of memory, losing the use of my right hand, and not being able to stay focused due to stroke. I apologize for this email turning out to be longer than I had planned, but that’s as close to a nut shell as I could get…I appreciate your time and any answer you have for me..in lamens terms please.
Thank you,
MaryAnn
MaryAnn, I’m not sure what the question is, but for liability and professional reasons I cannot offer personal medication advise in the forum.
Jeffrey Fudin, I was wondering if, it is “by law” for a physician to check a persons heart condition while on methadone, or any other pain medications. As a patient, we have to sign a contract to receive the medicine, but what does the physician actually guarantee the patient? Other than writing the prescription, I feel he/she should also be obligated to check heart and lungs on a regular basis…considering the side effects these meds give. Especially when someone complains of sharp pain in their right arm, and loss of ability to use that hand immediately following. As a patient, I had always thought signs of heart attack or stroke was in the “left” arm, but, a doctor should know that it “is” common for women to have that pain in the right arm…So many silent strokes could have been avoided if they would have done an ekg, or even sent me to a cardiologist “just in case”…Does the physician have no responsibilities to protect the patient on methadone? I understand if you cannot answer, I just think there shoulld be a general list of things drs should check for- each and every visit -when the patients medication “can” cause strokes & heart attacks. It doesn’t sound fair that we, as patients, pay good rates for such poor work..I won’t name the facility, but, had they been a plumber..I would have fired them in a heart beat. Unfortunately when taking drugs that make you drowsy, you don’t think clearly enough, and rely upon the dr’s to watch over you a little more closely… Dr.s these days are overloading themselves with patients for the money, and therefore have 3 or 4 nurse practitioners doing the work ‘for them’, and no way can keep up with proper care for their patients, or even making themselves aware of what they are experiencing. I “do” however appreciate your quick response to my message.
Maryanne,
You bring up some interesting points. No, there is no legal requirement to dictate specifically “for a physician to check a persons heart condition while on methadone”. Please read the FDA “Information for Healthcare Professionals Methadone Hydrochloride” which I have linked for you.
Mary Ann, yes if you are on Methadone for pain management, you need an EKG at least every 6 mos. Methadone can effect you heart. It is a risk usually with higher doses, but it is the responsibility of your Pain Dr. to order periodic EKG’s. Thankfully you are now. being treated by a competent pain clinic and Staff.
There is no legal requirement for a physician to do an ecg when the patient is on Methadone.
Yet the following post says you should have an ecg every 6 months at a pain clinic.
I had a pain clinic do ecg’s on me when my Methadone dose was increased from 2.5 mg twice per day to three times per day. The pain clinic PA would say oh, this ecg is much better than the other.
You can see how the knowledge of ecg’s was lacking at this pain clinic. My cardiologist said the ecg is either normal or abnormal. I have never had an abnormal ecg.
When I saw the np, she said she could not increase the Methadone dose to 3 times per day as my qt interval was 399, as though the Methadone was responsible. In fact, one study found ecg qt interval results were “all over the place”
The pain clinic i went to said “we want you off your methadone”. I have taken Methadone for 12 years, near same dose between 2.5 mg. 3x day or 5 mg. 3 x day.
But the CDC report on Methadone makes it sound pretty scary as though it was causing overdose deaths. Later, the CDC clarified the Methadone deaths were not representative of the general population but a group who received Methadone Maintenance therapy Further, the CDC did not talk talk about mixing Methadone with alcohol and the overdoses from that with with mixing other drugs as well. The CDC wrote to me saying their guideline were for primary docs. Their guideline were not talked about for pain physicians. But some pain physicians quote the CDC stats, some of those stats are just wrong, and they try to follow the CDC guidelines for chronic pain patients.
The CDC is at least partly responsible for the misunderstanding of Methadone and the guidelines were said to be biased.
It has cause problems for doctors and patients.
It became an opioid hysteria.
Hello Mary,
I hope that this gets to you. I am in chronic pain also. Broken back, twice, botched hip implant etc etc. My heart goes out to you. God i am sorry to hear that you have been through such an HORRIFIC living nightmare. My situation is the same only different. You seem to be doing all the”right” things but your treatment is in the hands of IDIOTS. I will pray that you come into contact with the right people/person that can turn your impending train wreck around. I will PRAY for you. God bless you Mary.
With heartfelt regards,
Chip Hoy
Hi MaryAnn! I responded to this post for new to this page and didnt think to hit reply. Oops. So ifffff youre ever on here again, pls take the time to scroll above and check out my post by KERRYANN. THANKS
2165 Ramelli Ave.
I have been an intractable pain patient for over 15 years,I was first seeing a Dr. for about 3 years, untill he was busted for over prescribing. so now at that time I no longer had a Dr.! Several months later I ended up finding a wonderfull Dr. in Pamona, Ca. Long story short i was discharged for missing a appointment, due to the fact that I lived ,10 to 12 hrs.away, and had no money at the time for transportation!! I desperately need a dr. that can prescribe me methadone, because nothing else works!!! I live in the Oroville, Ca. area. I truly hope someone or somebody can help me find a Dr. that would be able to help me, and to also realize that methadoe is one of the best pain relivers1 Thank You