We have previously opined on appropriate use of naloxone in the hospice setting and the questionable policies of some nursing homes to disallow naloxone at the bedside of their residents. We have also discussed accessibility of naloxone in the U.S. as the FDA considers a transition naloxone from prescription-only status to over the counter (OTC). A recent inquiry regarding the utility of naloxone in patients taking tramadol recently sparked discussion among pharmacy colleagues regarding the generalizability of recommendations to provide naloxone to all patients on opioid therapy.
Here to discuss these issues on this important guest post is Dr. Amelia Persico and PharmD Candidate Youssef Bessada.
In a 2018 advisory, the U.S. Surgeon General stressed the importance of expanding the awareness and availability of naloxone as a key part of the public health response to the opioid epidemic. This includes increasing the targeted distribution of naloxone to patients at an elevated risk of opioid overdose in addition to patients taking opioids for long-term management of chronic pain1. The advisory defined four factors as placing patients at increased risk of opioid overdose; misusing prescription opioids or use of illicit opioids, having an opioid use disorder, being recently discharged from emergency medical care following an overdose, being recently released from incarceration with history of opioid misuse of opioid use disorder. It is noted that specific risk factors have been further identified in the literature and a statistically validated tool is available to calculate risk of opioid induced respiratory depression (RIOSORD).2
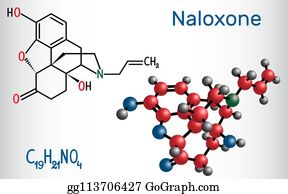
The utility of naloxone as an opioid reversal agent makes it a desirable medication to have on hand for patients on opioid pain therapy; particularly those at increased risk of opioid induced respiratory depression as described in the Surgeon General’s Advisory. However, naloxone’s utility and safety may not be generalizable across all opioids with consideration to atypical opioids, particularly partial agonist opioids such as tramadol. Tramadol, a phenylpropylamine, is approved by the Food and Drug Administration (FDA) for the management of moderate to moderately severe pain as a centrally acting synthetic opioid analgesic. Despite being officially switched from a Schedule V to a Schedule IV controlled substance due to its abuse potential in August of 2014, analgesia associated with tramadol use is only partially, and perhaps minimally attributed to mu-opioid agonist activity. Inhibition of the norepinephrine reuptake also contributes to the overall analgesic effect in the same way that SNRI antidepressants are effective in management of pain.3 Tramadol’s opioid activity is unique due to both low affinity binding of the parent compound (6,000 times less than that of morphine) and higher affinity binding of the O-desmethyl metabolite, M1, to mu-opioid receptors.4 As such, tramadol-induced analgesia is only partially antagonized by the opiate antagonist naloxone as has been proven in several animal studies situation.3
Tramadol’s serotonin and norepinephrine reuptake inhibitory effects result in a unique adverse effect profile. Increased blood pressure and heart rate have been observed owing to the increased sympathetic tone associated with noradrenergic activity. In addition, patients prescribed tramadol are at increased risk of serotonin syndrome and seizures. Risk of seizures increases with higher doses of the medication and concomitant use of medications that increase serotonin in the synaptic cleft (SSRI antidepressants). This risk is further potentiated with naloxone administration in an overdose situation, which as warned in the tramadol FDA package insert. “Abrupt postoperative reversal of opioid depression after using naloxone may result tremulousness, tachycardia and seizures”.5 Since naloxone carries a small seizure risk on its own, combining it with tramadol may further lowers the seizure threshold. This combination has potential to induce a seizure particularly in a patient at elevated risk of serotonin syndrome. A study by Lagard et al in the Journal of Clinical Toxicology in 2018 found that while naloxone reversed tramadol-induced respiratory depression (p < .05) in Sprague-Dawley rats overdosed on tramadol, it significantly increased seizures (p < .01) and prolonged their occurrence time.6
According to the World Health Organization, very few cases of tramadol-related severe respiratory depression have been described in the literature. The cases described all concern cases of overdose, while at therapeutic doses, tramadol produced less respiratory depression, both in adults and in children, compared to morphine, pethidine, and oxycodone.7 It is important to note that the utility of naloxone in the setting of poly-substance overdose, particularly with more potent mu-opioid agonists, remains.
Naloxone is generally considered to be a safe reversal agent to a suspected overdose and a lifesaving tool to have in our armamentarium as health care providers. However, given tramadol’s pharmacological make-up as a partial opioid agonist with low binding affinity to the mu-opioid receptor, it may provide little benefit in the setting of tramadol overdose. This small effect coupled with an increased, albeit low, risk of seizures in a tramadol-induced overdose may be a situation where potential risks outweigh the benefits and that there is poor rationale to support the common co-dispensing of naloxone with tramadol.
We are particularly interested in comments and discussion from our colleagues!
Youssef Bessada is a PharmD candidate in the class of 2020 at Albany College of Pharmacy and Health Sciences in Albany, NY. He is currently completing an advanced pharmacy practice experience in Pain Management at the Stratton VA Medical Center. After graduation, he plans to complete a PGY-1 residency, with interests in ambulatory care pharmacy and cardiology.
Dr. Persico graduated from Union Graduate College with an MBA in healthcare management in 2016 and completed her doctor of pharmacy at Albany College of Pharmacy and Health Sciences in 2017. She is currently a PGY2 Pain and Palliative Care Pharmacy Resident at the Stratton VA Medical Center in Albany, New York
References
Office of the Surgeon General. U.S. Surgeon General’s Advisory on Naloxone and Opioid Overdose [Internet]. 2018 [cited 2020 Feb 12]. Available from:https://www.hhs.gov/surgeongeneral/priorities/opioids-and-addiction/naloxone-advisory/index.html
- Zedler B, Xie L, Wang L, Joyce A, Vick C, Brigham J, Kariburyo F, Baser O, Murrelle L. Development of a Risk Index for Serious Prescription Opioid-Induced Respiratory Depression or Overdose in Veterans’ Health Administration Patients. Pain Med. 2015 Aug;16(8):1566-79.
- ULTRAM oral tablets, tramadol HCl oral tablets [package insert]. Titusville, NJ: Janssen Pharmaceuticals Inc; 2019
- Fudin J, Boglish P. Ask the expert: is tapentadol a glorified tramadol. Practical Pain Management. 2016 Jan;16(1).
- NARCAN(R) nasal spray, naloxone HCl nasal spray [package insert]. Radnor, PA: Adapt Pharma, Inc; 2017
- Lagard C, Malissin I, Indja W, Risède P, Chevillard L, Mégarbane B. Is naloxone the best antidote to reverse tramadol-induced neuro-respiratory toxicity in overdose? An experimental investigation in the rat. Clin Toxicol (Phila). 2018 Aug;56(8):737-743.
- World Health Organization. Tramadol: update review report – agenda item 6.1 [Internet]. 2014 [cited 2020 Feb 14]. Available from: https://www.who.int/medicines/areas/quality_safety/6_1_Update.pdf



The mu opioid activity of tramadol has never attracted much attention until the re-scheduling of the product by the FDA. I have used tramadol for breakthrough pain w patients on OUD levels of buprenorphine therapy for several years despite the low probability of mu opioid analgesia with competing receptor site occupation. Withdrawal symptoms from the SSRI/SNRI molecules is more challenging to manage and presents clinically more often than tramadol related adverse effects. Seizure activity with tramadol has also observed in patients with any compromised blood brain barrier (i.e. TBI and stroke). I appreciate the insights as to the pharmacodynamics of tramadol and naloxone which support the observations above.
Thank you Karen!
Great writeup Amelia and Youssef. I agree that when taken as prescribed, and as the sole respiratory depressant causing agent, tramadol has a very low potential for clinically relevant respiratory depression. However, in my population, it is not uncommon to find other (nonprescribed) opioids, benzodiazepines, sleep hypnotics, etc. in urine drug screens. These are the patients we need to be concerned about as well as rapid metabolizers of CYP 2D6 given the significantly higher MOR agonist activity of O-desmethyltramadol. As a routine practice, perhaps co-prescribing naloxone with tramadol isn’t rationale, but from a harm reduction standpoint, it puts naloxone in the home of patients with a higher than general population risk for opioid / polypharmacy overdose.
For those truly interested in this topic, I strongly encourage reviewing reference #6 from this nicely written blog.
Dr. Herndon; Thank you for your thoughtful comments!
It’s a matter of ABC. If a patient is not breathing, and an overdose of an opioid is suspected, the clinician rescuing the patient must first open the (A) airway and then provide for adequate exchange of air (oxygen), i.e. (B) breathing. If this can be done with some manner of artificial respiration then the need for naloxone is not primary. If, however, the person providing the rescue services is either unable to or unwilling to provide rescue breathing, then naloxone treatment is warranted. Serotonin syndrome and seizures can be life threatening, but they are both treatable. By contrast, “not breathing” always ends in death. Thus, with patients on tramadol who are at increased risk for opioid induced respiratory compromise, in the appropriate environment I see no problem with allowing them access to naloxone for emergency use
Addendum. Here’s what the package insert says and I am in agreement:
“Respiratory Depression Administer tramadol hydrochloride extended-release capsules cautiously in patients at risk for respiratory depression. In these patients alternative non-opioid analgesics should be considered. If large doses of tramadol are administered with anesthetic medications or alcohol, respiratory depression may result. Respiratory depression should be treated as an overdose. If naloxone is to be administered, use cautiously because it may precipitate seizures”
Thank you James!
Tramadol was not even a scheduled drug a few years ago due to it’s weakness. Even mentioning that naloxone needs to be co-prescribed is laughable.
What is a concern is that physicians that could not make it into mainstream medicine are trying to influence legislation is even more laughable.
Sorry, but that’s the way it is.
Tim Mason
Pharma Research Chemist