Happy New Year CMS, Buprenorphine and Tapentadol
As many of you already know, the Centers for Medicare & Medicaid Services (CMS) has established new policies that will be implemented January 1, 2019 around opioid prescribing. They call this their “three-pronged approach to combating the opioid epidemic” and it includes the following:
- prevention of new cases of opioid use disorder (OUD)
- treatment of patients who have already become dependent on or addicted to opioids; and
- utilization of data from across the country to better target prevention and treatment activities.
The imperceptiveness of “…strengthen and broaden our partnership with providers” is uncanny to say the least. More likely than not, this new policy will drive a wedge between dispensing pharmacists and prescribing clinicians with the heart of long-term opioid patients square in the middle of a sharp blade.
According to their Prescriber’s Guide to the New Medicare Part D Opioid Overutilization Policies for 2019, available HERE, through their “2019 Medicare Part D opioid overutilization initiatives, CMS seeks to strengthen and broaden our partnership with providers to address the opioid crisis.”
With clearly diminished opioid prescribing and dose reduction in almost every state, we’ve seen consistent rises in opioid deaths; some by suicide of suffering patients; some from legitimate patients seeking illicit opioids because they are unable to obtain them from their medical provider; and some from addicts who are overdosing on heroin laced with fentanyl analogues (not to be confused with pharmaceutical fentanyl).
To review, here’s what the new policies will require, copied directly from the above link…
Specific to prescription opioids, beginning in January 2019, Medicare Part D plans will employ the following new safety alerts at the pharmacy:
7-day supply limit for opioid naïve patients: Part D plans are expected to implement a hard safety edit to limit initial dispensing to a supply of 7 days or less. A hard safety edit stops the pharmacy from processing a prescription until an override is entered or authorized by the plan.
CMS’ goal with this policy is to reduce the potential for chronic opioid misuse through closer management of opioid naïve patients. Clinical evidence cited by the Centers for Disease Control and Prevention (CDC) found that opioid use for acute pain is associated with long-term opioid use and that a greater amount of early opioid exposure is associated with greater risk for long-term use. Recommendation 6 of the CDC Guideline states that opioids prescribed for acute pain should be limited to 3 days or fewer, and that more than a 7-day supply is rarely necessary. Limiting the amount dispensed with the first opioid prescription may reduce the risk of patients developing a future dependency or overuse of these drugs.
A pharmacist can dispense partial quantities of an opioid prescription consistent with state and federal regulations. However, if a prescriber believes that an opioid naïve patient will need more than a 7-day supply initially, the provider can proactively request a coverage determination on behalf of the patient attesting to the medical need for a supply greater than 7 days. Additionally, if a provider assesses upon re-evaluation that a patient will need additional opioid therapy, subsequent prescriptions will not be subject to the 7-day supply limit, as the patient will no longer be considered opioid naive.
Opioid care coordination alert: This policy will affect Medicare patients when they present an opioid prescription at the pharmacy and their cumulative morphine milligram equivalent (MME) per day across all of their opioid prescription(s) reaches or exceeds 90 MME. Regardless of whether individual prescription(s) are written below the threshold, the alert will be triggered by the fill of the prescription that reaches the cumulative threshold of 90 MME or greater. It is the prescriber who writes the prescription that triggers the alert who will be contacted by the pharmacy even if that prescription itself is below the 90 MME threshold.
This safety alert includes a 90 MME threshold for identifying potentially high risk patients who may benefit from closer monitoring and care coordination. 90 MME is cited in the CDC Guideline as the level above which prescribers should generally avoid. This is not a prescribing limit. In reviewing the alert, the pharmacist may need to consult with the prescriber to confirm medical need for the higher MME. The pharmacist can then indicate that the prescriber was consulted so the prescription claim can pay.
The care coordination safety alert is a proactive step to give prescribers more information, and if warranted, to encourage prescribers to emphasize opioid overdose risk and prevention with their patients, especially if the patient is receiving prescription opioids from multiple prescribers or pharmacies.
Will the pharmacy call the provider every time a patient has an opioid prescription that reaches or exceeds 90 MME for the care coordination safety alert?
No. The provider will be initially contacted by the pharmacist if a patient presents to the pharmacy with a prescription that reaches a cumulative threshold of 90 MME or greater across all of the patient’s opioid prescriptions and triggers the alert at the pharmacy. Once a pharmacist consults with a prescriber on a patient’s prescription for a plan year, the pharmacist does not have to consult with the prescriber on every opioid prescription written for the same patient after that unless the plan implements further restrictions. For example, Part D plans also have the option to set an additional alert that stops a prescription from being filled at the pharmacy if the opioid threshold reaches 200 MME or greater and may additionally include prescriber and pharmacy counts.
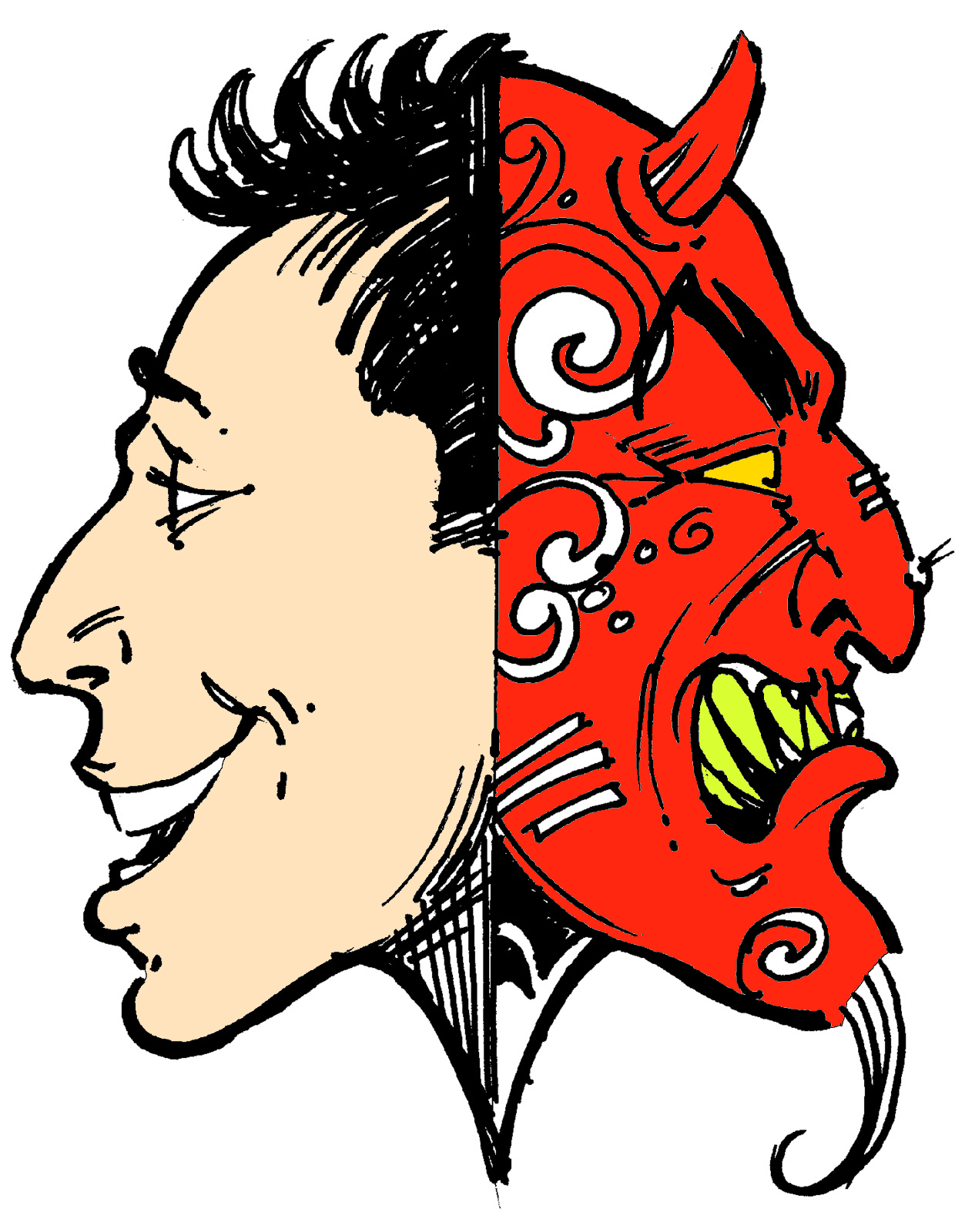
There are of course many issues here. The statement “For example, Part D plans also have the option to set an additional alert that stops a prescription from being filled…” concerns me because I believe that insurance providers that partner with Medicare will exercise carte blanche and treat this as an avenue to halt coverage on any opioids more expensive than the more abusable generics; I suspect they will attempt to limit payment for or require higher copays for many of the extended release opioids, abuse deterrent formulations, buprenorphine, and tapentadol. Pharma will likely respond with direct to patient discount cards, and will be forced to deal with the devil, PBMs to gain favor for coverage.
Prescribers and pharmacists will likely not have the time to duck patient care responsibilities to make these calls to each other, and if they try, experience tells me it will be a game of telephone tag. Both pharmacists and prescribers will likely avoid prior authorizations at all costs which will result in drastically lowered opioid dosing and rapid tapering, as covered in a previous blog, If You are Forced to Stop Opioids. Regarding the 7-day limitation, I believe that, in many cases, by the time a prior authorization is approved for opioids beyond the 7-day limit, the acute pain phase will likely have passed, unless CMS mandates that their private sector contracted insurance providers have a quick turnaround with implemented penalties to the insurers – don’t hold your breath.
CMS should mandate that insurance carriers not disincentivize (by requiring higher copays) or reject buprenrophine (Belbuca and Butrans) in favor of any full agonist opioid for new patients just because of cost. I have seen many insurance companies deny these in lieu of full agonist opioids (including morphine, methadone, fentanyl transdermal, and others). Where’s the forthright safety concern there?
In fact, a previous blog, Insurance Companies, Learned Helplessness, and Opioid Deaths, outlined one example of a real case where tramadol ER was rejected in favor of first failing methadone, morphine ER, or Oxycodone ER. I wonder if failing these drugs includes death.
Since CMS refers to the CDC Guidelines as a gospel of sorts, they should also require that tapentadol (Nucynta) be a formulary item and prescribed in advance of traditional full agonist opioids, at least for chronic pain. In fact, the CDC’s CALCULATING TOTAL DAILY DOSE OF OPIOIDS FOR SAFER DOSAGE makes no mention of an MME for either buprenorphine or tapentadol, and for good reason… There isn’t one. For more info on that, see Academy of Integrative Pain Medicine’s White Paper, Opioid Dosing Policy: Pharmacological Considerations Regarding Equianalgesic Dosing which clearly delineates the fallacy of morphine daily equivalents, especially with buprenorphine and tapentadol.
If all other non-opioid options and non-medication alternatives have been exhausted, and a careful, rational decision has been made to begin opioids following risk stratification, my recommendation to providers that want to stay off the CMS morphine milligram equivalent (MME) radar for new patients requiring long-term opioid therapy is to start with buprenorphine first because it has a ceiling effect on CO2 accumulation. It also disallows full agonist opioids to hog up mu-receptors, and once buprenorphine occupies those receptors, it is difficult for the full agonist to find an unoccupied mu-opioid receptor. Buprenorphine in that regard is like a game of musical chairs, where all chairs (aka mu-receptors) are occupied by buprenorphine, and the person that gets bumped when the music stops is the full agonist opioid. For this reason, buprenorphine overtakes the receptors but can still offer analgesia similar to or better than the full agonists being displaced. Next choice is tapentadol because the dual mechanism offers excellent analgesia at a finite dose with reduced toxicity. Only after these should a traditional full agonist opioid ever be considered, and if CMS is really concerned about misuse, an abuse deterrent formulation should be favored – this won’t happen if CMS allows their contracted providers to implement their own rules, as is this case now. Afterall, the new CMS policy upfront and center sates, as seen in #1 above, “prevention of new cases of opioid use disorder (OUD)”. Assuming that CMS is actually troubled about safety, they should include this as part of their policy. Moreover, in terms of safety, the CDC Guidelines encourage the use of in-home naloxone, especially when titrating or converting from one or more opioids to another. Where is the CMS recommendation of a requirement to provide, train, and pay for FDA approved in-home naloxone? Surely if they are mostly concerned about safety over cost, this should be included in the new policy, right?
I am fervently in favor of opioid policies that are evidence-based and will transparently improve safety. I believe that the new CMS policy, while presumably well-intended, will make the opioid crisis worse both in terms of opioid-related deaths (legal and illicit) and for patients that truly require long-term opioid therapy that will end up bedridden, depressed, and suicidal.
I usually would close this by wishing all of you a Healthy and Happy New Year, and although I do wish this for all our readers, good luck with that!
As always, comments are welcome!

Dr Fudin :I need all the help I can get on potential pallative care. Can explain on facebook Joe white …… E -mail below….
It makes no difference to my pain management doctor that palliative care is excluded. He blamed these policies for taking me off the medication that has been a godsend for me [and preauthorized by my insurance for 10 years].
He had no problem prescribing tapentadol even though I had trouble breathing with it. Take it or leave it, as if it’s the only pain medication on Earth. I need relief but I also need to breathe so I canceled the prescription and the upcoming appointments. I’m looking for a new doctor since last week but it’s not looking very good. .
Thank you Dr Fudin,
The support pain patients have gotten from so many doctors, PhD’s, scientists and Professionals of all colors is very heartwarming. We, pain patients are in your debt for eternity. There are so many of us that are completely gone and hopeless, many don’t know what to do or where to turn. I joined a group called mychronicpainteam, all the pain patients in this group had no idea how to fight back and advocate for themselves, within 1 week the monitors kicked me out of the group because I kept promoting websites like the national pain report. These people were hungry to learn how to fight back. We need pain patients that CAN, to stand up and fight for their rights and the rights of their doctors to be left alone, not falsely accused of being a pill pusher. It’s time to put medicine back in our doctor’s hands. I could go on all day.
Thank you again for posting this Dr Fudin!
Happy New Year
David W Cole
I have posted the chronic care codes info on my Twitter feed for those whose states do not have defined palliative care programs. Physicians can use these as documentation of medical necessity when there are two or more medical conditions that require integrated care which includes pain management.
Thank you @tal7291. This is great!!!
Thank you Terri,
I only wish we had a million of you out here!
Mr Lewis: and to Dr. Fudin; Thank you I need all the help I can get : I can explain @ joawhite60@gmail.com
Just found this. They must have just added it.
This is in addition to previous email.
CMS.gov has added 3 new downloads
that are chuck-full of information for
the patient, pharmacist, and prescribers.
https://www.cms.gov/Medicare/Prescription-Drug-coverage/PrescriptionDrugCovContra/RxUtilization.html
DOWNLOAD THESE 3…….
“Information for Patients”
“Information for pharmacists”
“Information for prescribers”
Richard, you are the man!!!
At CMS.gov you can click on this link.
https://www.cms.gov/Medicare/Prescription-Drug-coverage/PrescriptionDrugCovContra/RxUtilization.html
Then under downloads,click on this for Oct 23rd 2018 memo to Part-D sponsors.
Medicare-PartD-Overutilization-Control-HPMS-memos (October 2018)
Personally, I think every doctors office should have a copy of this
memo on hand. And every patient on opioid prescriptions.
The one thing we know for sure, is we don’t know for sure
what is going to happen after Jan. 1. This memo “should” help
clarify some things. Patients should be getting Prior. Auth. for their
opioid pain meds NOW. That may be helpful.
What I can tell you from my own experiences in the Las Vegas valley area
is this: 3 pharmacists, one from Walmart, Smiths, CVS, know NOTHING
about the new safety edits. They already call the doctor’s office for
any Rx’s at 50MME or above. So anything from 90MME to 199MME
will not cause an increase in pharmacists calling doctors. As a soft edit,
they will confirm intent once, put in an over-ride code and fill the Rx.
(in a perfect world)
I emailed 20 contacts listed from the CMS web site who are designated
opioid-overutiliztion contacts. Contact them to ask questions. None
replied to my emails.
In our area, for part-d plans, Aetna is the most inexpensive insurer and
probably will get most of the patients. I have talked with a total of 7
representatives, 3 in coverage determination/prior. auth. NONE of them
knew anything about the new opioid rules for part-d plans. I got a prior.
auth. for one Rx for 2019. They did a test to see if it would go thru ok and it did.
Paid for as usual. And it did not cough out ANY safety edits.
From the Oct. 23rd memo, I include my own thoughts about
what it means. If this memo can be used against any insurer,
then it should.
Hard edits at 200MME or > are probably going to be the biggest problem.
— What to do? again be proactive with prior auth. or coverage determination,
After Jan. Be Prepared.
— be able to quote the 2019 Call Letter, who is excluded i.e. palliative care
— be able to quote the Oct 23rd CMS Newsletter to all part d sponsors.
For instance, on page 3, the 200MME edit “is NOT a prescription limit”
on page 3, if MME is the only thing being questioned, the
attestation that the daily dose is medically necessary is suppose
to be all that is needed for patient exemption.
on page 3, after attesting medical necessity, the plan cannot ask
for additional requirements IE: a “pain contract”
on page 8, it reiterates this, you do not need a pain MGT. consult,
or pain contract, or a treatment plan. And repeated again, a simple
attestation that Rx’s are medically necessary is sufficient.
On page 7, Who should be excluded? Long term care facility, hospice, palliative care,
end-of-life, and active Cancer. (I’d also include residual post CA pain myself)
Also excluded, previously determined pain patients, those with a past history,
previous coverage determinations, prior auth., and prior auth. by case MGT
and/or appeal process.
As I said, the only thing for sure, is we don’t know squat about what will
actually happen. But everyone can try to be prepared.
Thank you Richard. This is fabulous!!! It’s nice to know that one of my peeps is in top of this! Kudos you and great for your patients!!!
Long time listener, first time caller – Great perspective Dr. Fudin – I agree and have experienced similar situations of un-intuitive coverage decisions while claiming “safety first”
Thank you Dr. Fudin. It goes without saying that this is more tragic news for the chronic pain patients and sadly appears as though it will do little to nothing to achieve the stated goal of “safety”. However, as you’ve so aptly stated may well, in fact, contribute greatly to the continued rise in both overdoses and suicides as more prescribers choose forced tapering. Safety cannot not be the true goal here when CMS relies on the CDC’s Guideline for its evidence after these have been proven to be dangerously flawed and clearly denounced by even its own authors.
This should be filed in your library of important columns on CMS prescribing policies. The Law of Unintended Consequences always applies when government interventions are not thoroughly vetted. Here is an example.
The start of a Happy New Year? Thanks
Thank you so much as always Dr. Fudin!