Dr. Raouf just can’t get enough pain! Thank you for sharing your insight as a full fledged PharmD. Here’s what Dr. Raouf has to share…
How often do we see a patient filling the same “oxycodone/APAP 10/325mg 1 tablet PO Q4-6 hours PRN” every month that was started years ago? If your answer is “Yes”, then this blog is for you.
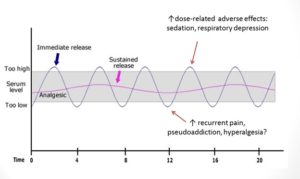
Opioids have a narrow therapeutic index and wide interindividual variability. Fluctuations in serum levels could result in toxicity or lack of efficacy. Immediate-release (IR) opioids are rapidly absorbed into the blood stream and have shorter half-life compared to ER. While this may be great for management of acute pain, it may not optimal for long-term management of chronic pain, which is defined as pain lasting for more than 12 weeks. 1
So back to the original question: “How often do we see a patient filling the same “oxycodone/APAP 10/325mg 1 tablet PO Q4-6 hours PRN” every month that was started years ago? So what are the problems here? Let’s start out by naming a few:
- Recurrent pain: the troughs associated with wearing off of the opioid result in increased neuronal firing and pain sensation. Patients often describe that the medication works “great” when they take it but the pain “comes back with vengeance” a couple of hours after. This could be due to the “fast on fast off” effect with IR opioids.
- Pseudo-addiction: defined as “drug-seeking behavior that simulates true addiction, which occurs in patients with pain who are receiving inadequate pain medication”.2 Pseudoaddicted patients become preoccupied with finding their opioids and attempt to refill them early in anticipated fear of running out. Pseudo-addiction is iatrogenic syndrome that is often a result of frequent ‘recurrent pain’ mentioned previously.3 They are “branded” as “drug seekers” where they are trying to find pain relief.
- Hyperalgesia: opioid-induced hyperalgesia (OIH) is a paradoxical response to opioid administration that results in increased pain sensitivity.4 Although not fully understood, hyperalgesia appears to be dose related. Rodent studies have demonstrated increased motor excitation, allodynia, and hyperalgesia with high dose morphine administration.5,6
- Toxicity: opioid-related adverse effects such as sedation and toxicities including serious respiratory depression are dose-related. 7-9 The higher maximum serum levels associated with IR opioids result in a higher risk for complications. But if this is the case why are there more cases of overdose with extended-release opioids? ER opioids are more attractive to drug abusers as they contain higher concentrations of the drug that is intended to release over extended periodic of time. When manipulated, their ER profile is defeated and they release the drug rapidly mimicking an IR formulation; however, they are releasing a higher, perhaps more concentrated weight/weight dose.
Figure 1: Immediate Release vs. Extended-Release Pharmacokinetic
Click HERE for enlarged PDF figure.
Minimum Effective Concentration
The concept of minimum effective concentration (MEC) for opioids has been established. MEC is the minimum concentration of an opioid to achieve pain relief. 11
What if pain had a minimum inhibitory concentration (MIC)?
Consider vancomycin or aminoglycosides where higher peaks/troughs are associated with nephrotoxicity and ototoxicity and lower troughs are associated with resistance. Metaphorically speaking, these higher peaks of opioids are associated with dose-related sedation and respiratory depression where the lower troughs are associated with recurrent pain, pseudo-addiction, and potentially increased tolerance and hyperalgesia with long-term use. Unlike vancomycin or aminoglycosides where there are pre-determined target MIC, the MEC for opioids varies from one person to another. As a matter of fact, MEC could change overtime within the same individual as they become more tolerant to the opioid and/or their pain-related physiology progresses.12
But My Patient Said Oxycodone/APAP Works Better and Refused long-acting Opioids
The faster a drug is released into the bloodstream and reaches the brain, the more euphoria or likability is associated with it. This feeling of euphoria may be mistaken for pain control as patient may report that the IR formulation makes them feel great that formulations associated with less euphoria are not effective in that regards. Patients may often express this by saying “it helps take my mind off the pain” “takes the edge off’. Patients are often unaware of this and it is our role as healthcare professionals to provide the corresponding education.
ER Opioids Patient Selection
As labeled by the FDA, nearly all commercially available ER opioids carry the indication of “management of moderate to severe pain when a continuous, around-the-clock analgesic is needed for an extended period of time”.13 ER opioids should only be used in opioid tolerant patients who have chronic pain. Opioid tolerance is defined as patients already taking at least 60 mg of oral morphine daily, 25 mcg transdermal fentanyl per hour, 30 mg of oral oxycodone daily, 8 mg oral hydromorphone daily, 25 mg of oral oxymorphone daily, or equivalent dose of another opioid for ≥7 days.14 ER opioids should not be initiated in opioid naïve patients. Patients with chronic pain defined as pain lasting for 12 weeks1 or longer may be suitable candidate for ER opioids.
There are various strategies on switching patients from IR to ER opioids depending on their pain control and tolerability of their current regimen. First, it is important to calculate patients total daily dose by asking the patient how often they are taking it rather than solely relying on the prescription label. Patients could be converted to ER opioid at 50-75% of their current dose with 10-25% IR allowance for breakthrough pain and titrated based on efficacy and safety.
Patient Case:
Patient with chronic pain secondary to degenerative disk disease and status has been on opioids for 8 months. His pain regimen includes oxycodone/acetaminophen 10/325mg orally every 4 hours as needed (patient reported taking 6 tablets/day). He is not a surgical candidate and is unable to take NSAIDs.
Step 1: Determine if patient a candidate for ER opioids:
- Patient meets the definition of opioid tolerance: ≥60 mg MEDD for ≥7 days
- Patient meets the criteria for chronic pain: pain lasing ≥ 12 weeks and his pain is likely to require chronic opioids
Step 2: Calculate total daily dose: 10mg oxycodone x 6 tablets = 60mg oxycodone/day (equivalent to 90 mg morphine per day)
Step 3: convert patient to an ER opioid at 50-75% of current MEDD. Potential opioids include:
- OxyContin (oxycodone ER) 15-20mg by mouth every 12 hours
- MS Contin (morphine sulfate ER) 15mg every 8 hours or 30mg every 12 hours
Step 4: Determine IR opioid allowance: Patient can take oxycodone/APAP 10/325mg once or twice a day as needed
Step 5: Monitor, evaluate, and titrate!!
Role of Abuse Deterrent Formulations
ER opioids usually contain higher amount of drug in a dosage form compared IR that is intended to be released over an extended period of time. When the integrity of the ER dosage form is disrupted either intentional for purposes drug abuse or unintentionally by a patient who unexpectedly crushes the medication for ease of swallowing, it behaves similar to IR formulations and release the drug more rapidly into bloodstream, thereby increasing risk for toxicity. There are abuse-deterrent formulations (ADF) discussed in our Pharmacy Times posts HERE and HERE, that have properties rendering them resistant to physical and chemical manipulations. Unfortunately, these are available as brand only and are either not covered by insurance or require a prior authorization process.
Chronic pain affects more than 100 million Americans and is projected to continue growing. Long-acting opioids are safe and effective for management of chronic pain when used appropriately. While it may seem more convenient to ‘just give patients a prescription for Norco, Percocet, or oxycodone/APAP each month, maintaining them on IR opioids long-term may not optimal and could come with various problems down the road as mentioned in this blog. It is important to understand and educate patients that the goal is to keep their pain at bay instead of chasing after it. Notwithstanding, there has been much chatter amongst various thought leaders that indeed extended release opioids do not allow the hypo-adrenal axis sufficient time to reset thereby elevating the risk of a hormone imbalance from ER opioids. – this remains to be seen and will require more study.
As previously mentioned in an article on Pharmacy Times by Drs. Throm et al, “The best analgesic results are obtained when a therapeutic alliance between the patient and health care professional is formed”
Dr. Raouf received his PharmD from Albany College of Pharmacy and Health Sciences, with a concentration in nephrology. He completed an advance practice rotation in pain management under the mentorship of Dr. Jeffrey Fudin at the Stratton VA Medical Center where he continued to volunteer thereafter as a student pharmacist. He has been involved in developing an automated software platform to assess pre-validated risk for opioid-induced respiratory depression to qualify patients for in-home naloxone. Dr. Raouf will be pursuing PGY-1 Pharmacy Practice Residency at the VA Tennessee Valley Healthcare System in June 2016.
References:
- National Institute of Health. Chronic Pain: Symptoms, Diagnosis, & Treatment. 2011; 6(1): 5-6.
- http://medical-dictionary.thefreedictionary.com/pseudoaddiction
- Weissman DE, Haddox JD. Opioid pseudoaddiction–an iatrogenic syndrome. Pain. 1989 Mar;36(3):363-
- Lee M, Silverman SM, Hansen H et al. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011 Mar-Apr;14(2):145-61.
- Yaksh TL, Harty GJ. Pharmacology of the allodynia in rats evoked by high dose intrathecal morphine. J Pharmacol Exp Ther. 1988 Feb;244(2):501-7.
- Kim J, Jung JI, Na HS et al. Effects of morphine on mechanical allodynia in a rat model of central neuropathic pain. Neuroreport. 2003 May 23;14(7):1017-20.
- Bouillon T, Bruhn J, Roepcke H, Hoeft A. Opioid-induced respiratory depression is associated with increased tidal volume variability. Eur J Anaesthesiol (2003) 20:127-33.
- Stambaugh JE, Reder RF, Stambaugh MD et al. Double-blind, randomized comparison of the analgesic and pharmacokinetic profiles of controlled- and immediate-release oral oxycodone in cancer pain patients. J Clin Pharmacol. 2001 May;41(5):500-6.
- Kaplan R1, Parris WC, Citron ML et al. Comparison of controlled-release and immediate-release oxycodone tablets in patients with cancer pain. J Clin Oncol. 1998 Oct;16(10):3230-7.
- http://learn.chm.msu.edu/painmanagement/pics/serumgraph.jpg
- Woodhouse A, Mather LE. The minimum effective concentration of opioids: a revisitation with patient controlled analgesia fentanyl. Reg Anesth Pain Med. 2000 May-Jun;25(3):259-67.
- Dumas EO, Pollack GM. Opioid Tolerance Development: A Pharmacokinetic/Pharmacodynamic Perspective. The AAPS Journal. 2008;10(4):537. doi:10.1208/s12248-008-9056-1.
- US Food and Drug Administration Questions and Answers: FDA approves a Risk Evaluation and Mitigation Strategy (REMS) for Extended-Release and Long-Acting (ER/LA) Opioid Analgesics. March 2013. Available from: http://www.fda.gov/Drugs/DrugSafety/InformationbyDrugClass/ucm309742.htm. Accessed May 5, 2016
- US Food and Drug Administration. Information for Healthcare Professionals: Fentanyl Transdermal System (marketed as Duragesic and generics) 12/21/2007 Update. Available from: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/DrugSafetyInformationforHeathcareProfessionals/ucm084307.htm. Accessed May 5, 2016.


Dr. Rauf,
I wish to suggest gently that your recommendations seem somewhat weakened by the fact that the entire methodology for determining Morphine Equivalent Daily Dose is highly suspect and largely arbitrary. See http://www.medscape.com/viewarticle/863477 “The Myth of Morphine Equivalent Daily Dose”.
As you point out, it is now known that patient sensitivity to various opioids is highly variable between individuals. This tends to confound treatment recommendations seriously. Likewise, there are no generally accepted studies of the effectiveness of either short term or long term release opioids in patients who take them for periods of years. Thus it is extremely difficult to generalize practice standards, even recognizing that drug tolerance and addiction are serious risks to be managed. Arguably, some of the problems that we observe in patients prescribed opioids may be attributable NOT to over-treatment, but rather to under-treatment of pain.
I write as a technically trained non-physician who has over 20 years supported and communicated with thousands of chronic neuropathic face pain patients. Among this population, a relatively small minority have failed all therapies other than opioids, and would face literally the loss of their quality of life if such medications are withdrawn — as they are being increasingly, since the March release of the CDC voluntary guidelines on prescription of opioids to adult non-cancer chronic pain patients.
Thus I must suggest that your approach is not only a hard sell, but it may in fact result in active harm to some patients.
Hi Richard,
Could you please elaborate on which approach you are referring to?
As for your comment on over-treatment or under-treatment if it is pertaining to the patient case, please review “Step 5: monitor, evaluate, and titrate”. For medications with narrow therapeutic index, it is important to start low and then titrate to safety/efficacy (First, do no harm). A safe starting point is to be followed by monitoring and appropriate titration. Of course these recommendations do not and can not apply to all situations as medicine is not a one size fits all, and with pain management, it is important to individualize therapy and constantly follow up with patients rather than using a fire-and-forget.
Most patients I speak with take an ER with IR for breakthrough pain. The fact is, 12 hour meds, do not 1. last 12 hours and 2. generally, need an IR med to help with breakthrough pain. Fact number 3. All of the meds a chronic pain patient takes, NEVER, get rid of the pain! This is the biggest misconception of the general public! When I am in the midst of a flare up, NOTHING, will touch the pain!
This really varies from one patient to the other. The published half-lives and duration of action for medications are the averages and there are outliers. When a patient reports consistently supplementing with an IR opioid on a daily basis as their ER doesn’t last, then it is time to re-evaluate their ER regimen and readjust accordingly. Depending on the opioid, some ER formulations can be used every 8 hours such as OxyContin and Ms Contin.
This is partially covered on PainDr.com in Hysingla & Zohydro: Same church different pew?
Let’s also consider fentanyl, there are patient who reports that the medication works well for 48 hours then the pain comes back. This does not apply to all opioids and it is important to check the package insert as Nucynta (Tapentadol) ER is true 12-hour dosing.
If I had a nickel for every time I’ve heard a pain patient say – “OxyContin isnt as effective as Percocet” – then I’d have more money than Martin Shkreli.
You’ve got a tough sell here guys, especially when convincing a new chronic painer whose pain is under control with IR meds, that ER opioids are in his/her best interest.
Therefore, please educate, titrate, and provide rescue dosing when rotating this person to ER meds.
Kurt,
We do agree on some of your points. I came across a patient who refused OxyContin and said that Percocet gives him a rush that takes his mind off the pain and his problems, and that he doesn’t get this effect with OxyContin. A big concern is if the patient attempts crushing OxyContin to yield the same euphoric effect: an honest mistake that could cost a life. That’s when education is critical especially on proper administration and the consequences of crushing it.
How DARE you write a blog suggesting that opioids are not “poison” for everyone?!?!?!?!
Great job, Jeff. Making good sense may make some zealots unhappy, however. 😉