As I write this post, I am sitting on a plane, row 26 in Atlanta, Georgia waiting for the aircraft door to close. Now that it’s closed, the 10 passengers immediately in front of me are sitting in two emergency exit rows. The flight attendant approaches them…
- Are you willing and physically able to assist in case of an emergency evacuation?
- Is everybody in rows 24 and 25 at least 15 years of age or older?
- Passengers nodding…
- I need a verbal response from each person individually…
- Yes, yes, yes, yes, yes
Now imagine entering your doctor’s office for a yearly physical. You have a diagnosis of hypertension (BP=170/97), diabetes (A1C=11), and heart disease (EF=32). Upon check-in with the receptionist, you are asked to sign a waiver.
- [Y] [N] I decline physical exam
- [Y] [N] I decline any discussion of risk factors
- [Y] [N] I decline any discussion of harm reduction and lifestyle modification including but not limited to diet, exercise, alternative treatment options or other
[Y] [N] I agree to renewal of my prescriptions without discussion or counseling
Here’s another example for pain patients…
- [Y] [N] I decline physical exam
- [Y] [N] I decline any discussion of pain level, ability to carry out activities of daily living
- [Y] [N] I decline any discussion of anxiety, depression, constipation, suicidal thoughts, or other
- [Y] [N] I decline any monitoring including but not limited to urine drug screens
- [Y] [N] I decline any discussion of harm reduction, risk of opioid-induced respiratory depression, alternative treatment options in addition to or instead of opioids, and lifestyle modification including but not limited to diet, exercise, or non-medication options
- [Y] [N] I agree to renewal of my prescriptions without discussion or counseling
#DitchTheDecline
Rewind to three days ago when I entered a local pharmacy for a prescription refill, albeit a non-opioid. As I approach a student pharmacist who didn’t know I was a pharmacist, as she handed me my medications, she asked me to sign the routine electronic pad, “[Y] [N] I decline counseling”. Although this has become the standard of care among community pharmacies, I couldn’t help but think, when did the train get off the track?
Today we find ourselves in an environment with politicians and mainstream media hurling blame at everybody and their brother for a presumed prescription opioid crisis. The FDA has ratcheted up their risk evaluation mitigation strategy (REMS) program to include immediate release opioids, and other strategic changes; state after state is requiring 3 or more mandatory hours of continuing education in order for clinicians to maintain their ability to prescribe controlled substances; several states and insurance carriers have placed limits on days supply of opioids for acute pain; Medicare has implemented a new program that will require hard and soft edits of morphine equivalent doses at the 90mg and 200mg marks, each requiring communication between pharmacist and prescriber (which could delay prescriptions for patients requiring chronic opioid therapy thereby precipitating withdrawal)… Need go on?
I’m pretty sure that the chance of my plane crashing is far less than the risk of accidental or intentional opioid 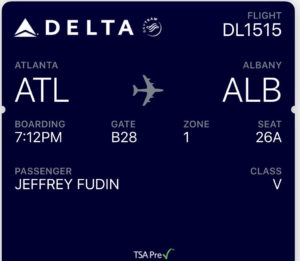 overdose, although we are experiencing significant turbulence at the moment which is making me second guess that. Yet, the stewardess needs to ensure the safety of passengers requiring a verbal affirmation from each that they understand the importance of their responsibility – although I feel like if we did crash, it wouldn’t make much difference – but the activity by this stewardess is standard practice and it’s mandatory!
overdose, although we are experiencing significant turbulence at the moment which is making me second guess that. Yet, the stewardess needs to ensure the safety of passengers requiring a verbal affirmation from each that they understand the importance of their responsibility – although I feel like if we did crash, it wouldn’t make much difference – but the activity by this stewardess is standard practice and it’s mandatory!
The clinicians above would not meet the standard of practice in either scenario above for the diabetic or pain patient, and the suboptimal attention could result in patient harm, death, and significant liability.
Nevertheless, somehow it has become okay, in fact the standard, for pharmacists to neglect an important duty to counsel. And why? Because we live in a profit-driven medical world where time is money and patients are inpatient, or believe that the pharmacist has nothing new to offer in terms of counseling.
Although it’s sad that it has come to this, federal and state law should eliminate the option for “declined counsel” for any controlled substances, opioids or otherwise. Why, because these medications by DEA definition have a high risk of abuse.
Examples of other Controlled Substances
- Amphetamines for ADHD: Remind parents that these are the most highly abused drugs among college students. Remind parents that these stunt growth in young children and it’s beneficial to take a drug holiday during winter, spring, and summer breaks so that your child can catch up on the growth curve.
- Testosterone supplements: Remind patient that there is elevated risk of anger and aggressive behavior, mood swings, and should not be used if predisposed to prostate cancer. Ask if anything has changed to elevate that risk.
You have long-term pain and require chronic opioid therapy, and don’t feel like you need counseling? A simple chat and a few reminders are not a bad thing each month and it certainly wouldn’t harm you.
Here’s how it should go…
Mr. Smith, I know you’re very familiar with your oxycodone, but I just want to take a few minutes to review some items to maximize safety and minimize potential side effects or other problems. Have you had regular bowel movements; is the consistency regular for you; do you feel like you’re straining or have incomplete evacuation? Have you changed your diet at all? Have you started any natural food supplements or any new diets; these things can elevate or reduce your opioid levels and cause pain or too much sedation. Do you feel like your pain is adequately controlled; if the answer is no, ask what the issues are. Is it a new pain or worsening of the old pain? Is it burning/shooting pain, or does it feel like bone pain or something else? Oh, it’s burning pain – you really don’t have any medications on board to specifically address that, but there are several options – you should make an appointment with your medical provider and discuss various options. Patient asks, such as what? Answer; certain antidepressants that are also indicated for pain that effect norepinephrine in nerves such as duloxetine; various anticonvulsants such as gabapentin and others; perhaps a switch to a different opioid that could add more benefit over oxycodone, but you should be to your doctor to determine if any of these are appropriate options considering your pain diagnosis and medical history. Are you able to do the same things now that you were able to accomplish 1, 3, or 6-months ago since your prescriber has reduced your opioids; how has that affected your mood and function; have you had withdrawal symptoms? How is your mood, your sleep?
You get the picture.
The role of a pharmacist has expanded exponentially over the last several decades. It is unacceptable to allow any patient to decline counseling for opioids. The counseling should not be demeaning or derogatory; instead it should be genuine, engaging, serious, caring, comforting, and helpful.
On a weekly basis I see various prescribers besieged for prescribing too much opioid, even in legitimate cases, criticized by regulatory agencies for not keeping pristine notes or appropriately counseling patients. Yet the very last hands through which the prescription passes have the legal (and standard-of-care) option of no note, no counseling, no preemptive safety discussions, or pep-talks, NOTHING.
At the risk of stirring up ill-feelings amongst my pharmacist colleagues and throwing my own peeps under the bus, it bothers me immensely to know that we can have a huge impact and also be a neutral advocate for patients and their prescribing clinicians. I know time is limited and that pharmacists are overworked. I also know that the physician time is limited and they are overworked. I know that too much time is spent by both of these professionals dealing with insurance payers to obtain prior approval authorizations for medications or procedures. I get it.
What I don’t get is how we can allow an innocent patient to “decline counseling” when it is our professional duty to keep patients safe and functional. We need a parachute for this decline in professionalism to help patients safely land instead of crashing and burning. Counseling should be the standard, and it should be mandatory! #DitchTheDecline
As always, comments are encouraged and welcome!


I would very much like for you to be my pharmacist. How can I arrange this ?
Andrea, I would love that. 🙂
Give me relocation directions and I’m THERE. ♥️
Wow!!! So it is not just me out there (in “here”) trying desperately to get the medications I NEED, not want! No on “wants” to have a truck use them as an off ramp So, for this patient….. alleged “epidemic” & how it’s being “addressed”…I always wonder, did even one authority think of the horrible human suffering that would spread out from this approach to America’s “opiate problem”? Because I knoe, after 20+ years….no one thought to ask any of Us. And we are Legion! Not religious but pain is a demon that will drive you over the edge.
Hi Jeff,
We created a community pharmacy advanced opioid counseling program which trains pharmacists in all areas of opioid counseling and helps identify patients at risk for respiratory depression with offer of naloxone. The education, created by UB, and the counseling checklist along with other materials are on our website: https://atlanticquality.org/initiatives/drug-safety/opioid-safety-com-pharmacy-intervention/
Thank you, Dr. Fudin, for this important and powerful message. This is definitely our duty as pharmacy interns or pharmacists, as we take the pharmacist’s oath “I will apply my knowledge, experience, and skills to the best of my ability to assure optimal outcomes for my patients.” If we just dispense medications to patients without counseling, how can we assure optimal outcomes for patients in terms of safety and efficacy (of any-and especially high alert-medications)?
Correct – you nailed it Mariam. It’s good to know that the future of pharmacy is in the hands of dedicated and thoughtful Interns.
I fully understand what the doctor wrote. What is bothersome for me about today’s practices is that any discussion regarding pain with a doctor should be carried out with the understanding that the doctor is going to want to know why he/she should prescribe pain medications, at all, especially narcotics. Most people have no idea of the risks. Counseling them should be mandatory from the outset. Periodic counseling should also be done when the medication must be continued.
My situation is not one of chronic pain, but one of intermittent severe pain that takes treatment and time before it typically resolves. Old injuries and messed up nerves plus old age make a difference. My PMD has refused to prescribe Tramadol 50 mg dosed at “one or two tablets q six hours PRN pain, in spite of the fact that he had done so before the FDA clamped down. I do have another doctor who will prescribe, but he will be retiring soon.
At this point, I distrust the FDA and the CDC for the havoc they have caused for patients who simply want to be able to live life without intractable pain — whether chronic or intermittent. They can analyze contrived statistics all they want, but they did not actual research in the field with actual patients. The CDC really was the wrong agency to bring into this. The failed efforts of the DEA are the major cause of this because there has been no slowdown of the illegal drugs entering the country. Addiction is not the problem with chronic pain patients. Addiction starts with a stupid decision. Pain patients do not choose to be in the situation they are in. They should not be punished based on statistics developed from addiction.
Cancer patients in the end stages of the disease should not have to beg for pain relief. People dealing with post-injury pain should not be denied pain relief. Patients dealing with health conditions that produce pain should not have to resort to Kratom (unregulated) to get relief. Insurance companies should not be dictating medical care at all.
I have been told that my situation is going to change and that the pain will become worse and constant. When that time comes, I have no hope for relief that way things are currently. I do not have the ability to travel for pain control. People without hope for relief do some very strange things…
Thanks Jeff! Another great post…and the patient responses are minimally reflective of the poor counseling ambiance in many retail pharmacies. It seems pharmacy counseling areas (or lack thereof) in general, go against what the pharmacy profession has been working so hard over decades to achieve – a better and more dynamic relationship with the patient. I guess that, in a perfect situation, (which I have seen) there would be a separate area or room around the corner from the prescription pick up line, upon filling a new prescription, the pharmacy technician would ask the patient to go to the counseling area/room where the pharmacist would meet him/her to discuss the new prescription…without the distractions of constant phone calls, insurance billing processing, prescription adjudication issues, the long line of people waiting to get their prescription filled while in earshot of counseling discussions, and demands of those in corporate pharmacies to process more prescriptions than time allows. Opioid prescriptions, in line with your blog, are a key therapeutic group of drugs I believe, along with many State regulations, should require counseling for new as well as refill prescriptions. As with many other therapeutic classes of medications, a few “focused” minutes discussing an opioid prescription and pain in relationship to activities of daily living (that can or cannot be performed), side effects, use of supplements or additional new prescriptions may, as your example indicates, lead to the discovery that an increase in the current opioid dose might be avoided with an alternate “non-opioid” medication specific to the type of pain discussed. Counseling/discussing prescriptions with people is an art that requires balance in communication and understanding of the patient’s given situation that results in a satisfying experience for the patient as well as for the pharmacist – so yes Jeff, I believe that in the area of counseling, and for so many internal reasons, the pharmacy train has gotten off the track.
My hat goes off to those individuals with chronic pain who, for decades, have been managed well by their medical practitioner and get their prescriptions filled by the neighborhood pharmacist who they’ve known for years and have a great professional relationship with – you are fortunate, as that is not the case for most.
You assume that pharamcies will fill the prescription and that doctors actually help pain patients. When my mother was alive (she passed 10/19 due to medical negligence) was on a reasonably low dose of pain meds for her shattered femur (PT abandoned her because of her pain and no one would do anything about it), and even though her doctor and her insurance company said the dose was a 15 day supply, when I went to fill it at Walmart, I was always a nervous wreck to see if this would be the time they cut my mom off, because THEIR guidelines trumped anything the doctor said.
For my own medication, I have severe chronic pain, 8-9 daily on the scale, and because the efficacy rate of Lyrica/gabapentin/Savella/Cymbalta hovers around the 35-40% rate for moderate to significant pain relief and those meds don’t work for me (fibromyalgia), I’m told to “suck it up and deal with it” even though I’m not looking for opioid pain medication. My blood pressure is extremely high and I have tachycardia because the pain doc told me he wouldn’t do anything until I was on at least 150mg of nortrapytaline a day, and yet, I can’t even get birth control pills because I’m a pain patient.
What I learned is that my life is disposable. The doctors taught us that my mother’s life was also disposable, and now you’re asking pharmacists to step in? How many more people have to die before you stop the genocide and criminalization fo pain patients?
Mary, I’m very sorry to hear about your misfortunes and difficulties. I’m guessing you’ve heard the expression, “Don’t bite the hand that feeds you”. An entire portion of my blog site has been dedicated to patients such as yourself, and questions are answered on my own time to help various people with pain -related medication issues. It is not helpful for you to lash out at me or anyone else because of your anger. I do hope things get better for you.
I had a CVS pharmacist refuse to fill an opiod script from my doctor in Detroit (live in KY). It was a script they had filled every month for over a year AND it was a decrease of the amount! He told me “to get a local doctor!” If I could have found one locally, do you not think I would??? I traveled 2 times a month 10 times for a full day in a hospital for treatment plus once a month follow up for 21 months until the doctor passed that no one locally had any clue! We spent lots of time and lots of out of pocket money to do this treatment. I would still do it today if the doctor was still alive! He literally saved my life and the life of our daughter who has had chronic Lyme for 20 years.
Monthly counseling does make sense if dose/schedule is changing, or if there’s a new diagnosis. But (except for pregnancy taper) I’ve been on the exact same dose of the exact same medication, for the exact same genetic condition, for 20 years. I know how to manage my diet the way that works for me, and never had side effects significant enough to seek medical attention. I really need to be asked about poop in front of my kid, every single month when we stop by the pharmacy?
Running errands with my kid, by the way, is something I can do because – thanks to medication – I’m not trapped in my house with refractory IC. The pharmacist already has important information about how I’m functioning, based on the fact that we’re out and about shopping, taking care of responsibilities, and living a normal life.
You must not be familiar with our medical visits that prelude the prescribed medication of opioids. And the important factor of extensive history and relationship with the doctor. An example of that is the doctor knows what medications you have tried and what did or didn’t work. The doctor and patient has a treatment plan to treat a disease he specializes in. Why would anyone take the pharmacist advice if it different from the treatment plan.or the doctors advice All the things you mentioned are gone over every month. I don’t feel that the pharmacist should expect a patient to go into detail again with them. There is no patient pharmacist confidentiality. Also, a lot of people are usually around so many wouldn’t share that information at the counseling window. I think if you went through being a pain patient for even a little bit you would understand how it’s totally unnecessary and what pain patients already go through to receive their medications.
Now that pharmacists are being asked to act as narcs and report so-called suspicious prescriptions, I am not volunteering any info. Some pharmacies are being asked to participate in Narxcare, how can we trust anyone, especially with such an insulting, volatile, judgmental name. I trust no one in the medical field to have the patient’s well-being in mind. They keep proving me right.
I appreciate the information being offered by Dr. Fudin. I had a converation with my doctor last month regarding the impact of reducing my MME dose. Apparently it doesn’t matter to the doctor. I subltely tried to get the point across that past reductions were intolerable and now wanting me to be on 90MME per day was not going to end well. You cannot expect someone in constant pain to live or be able to tolerate chronic pain. I read about the edit situation and it seems to me (if I am comprehending the statutes properly) my doctor and pharmacist can agree on a more helpful dose as long as they agree it is warranted and I am not at risk. 15 years of pain management without any problems (never any unprescribed medications found in my system and having the required tests, MRI, blood work) and not requesting unreasonable dosing should be enough for them to agree to adequately treat my pain. If the only requirement for going over the 90MME requirement is having the doctor write the prescription as required and confirming with the pharmacy that this is best for the patient, I am concerned why my doctor seems unwilling to take thses steps..
Because your doctor is scared to death of the DEA. All it takes is for their database to identify the number of prescriptions he writes as higher than the average in his area and they will be breaking down his door, seizing his patient records, closing his clinic, ruining his reputation and confiscating all of his assets. And they can do all of this without proving a single charge. So doctors are now claiming the CDC guidelines say they cannot write opioid prescriptions any more, even though the guidelines say no such thing. Your doctor would rather see you live in agonizing torturous pain for the rest of your life, or commit suicide, than risk everything he owns by continuing an opioid regimen.
So true!
I agree, in a perfect world pharmacists should be counseling patients on a regular basis. There have been a few instances where I was asked if I had any questions. Just the other day I picked up a new prescription and the pharmacist stopped what he was doing to come over to the drive thru window to explain what I could expect. This new one is different than anything I’ve taken in the past, and I was grateful to him for giving me a heads up. However, unless I have a question and ask specifically to speak to a pharmacist, the rest the time it’s just left up to the patient advisory leaflets that are stapled to the bag. I’ve never been asked by any pharmacist if a medication is actually working for me or if I’m experiencing any side effects. My pharmacy is very busy and usually has at least an hour wait, so I can also understand why they can’t/don’t counsel every patient on every prescription.
I don’t take opioids on a regular basis, so I’m not as concerned with that; but I am curious about how HIPAA and the rules for PHI play into counseling patients, especially when pharmacists are stuck behind a very busy, very public counter they can’t really leave and there’s usually a line of several people. A lot of what you mentioned above should most definitely be addressed, but I’m not sure how many people are comfortable with talking about their bathroom habits in public (as an example). It’s also concerning that someone looking for opioids may try to rob the customer after they leave the store if they hear and know a new prescription was just picked up. I’ve read of it happening although I’ll admit I don’t know how common it is. I don’t put anything past anyone, especially when they’re so hard to get legitimately now. I know some stores set up partitions in an attempt to protect identification, but those still aren’t private; Anyone standing in line can still hear every word.
I don’t know that there’s a good solution to this situation, unless private rooms are built in the pharmacies and there’s a pharmacist on duty dedicated to strictly counseling patients for the entirety of their shift. Most stores have more than one pharmacist employed, so maybe they could take turns between counseling and filling. However, I’m not sure stores would embrace this approach.
Along the same lines and something for your medical friends on this site to keep in mind, I’ve noticed more & more lately that doctors also seem to be talking a lot louder in patient rooms than they should be. Of course I realize that sometimes walls are thin, they’re usually in a hurry, and doctors try to go into rooms in a good mood for the most part – good mood sometimes translates into speaking louder, but I’ve heard just about every word of several peoples’ complete doctor visits in the last couple of months, and I’m sure other people have heard mine. It isn’t just at one particular doctor’s office either, but several. Just because patients may not see me walking out of the room or personally know who I am, that doesn’t mean that I want them to hear why I’m at the doctor and what’s going on with me. We still end up encountering each other at checkout, in the lab, in the parking lot, etc. I plan to politely bring this up at my next appointment(s) as well.
Mary, You are very perceptive. Yes, HIPAA guidelines most certainly apply and all pharmacies should have a separate counseling area. These regulations also vary by state in terms of a designated privacy area. Many pharmacies are starting to build separate rooms exactly as you suggest and those areas are being used to administer vaccines as well.
That’s encouraging, thank you. For now, mine just has a single partition wall with a chair behind it right up front at the end of the counter where they give flu shots. It’s off to the right side from the cash registers, but there’s only a few feet between the second register and the partition. Any counseling is done out in the open. The pharmacist will come down from the computer if you ask him/her to so you can speak in a softer voice, but I’ve also seen them answer questions out loud without leaving their spot in front of the computer multiple times. With some general questions, it doesn’t really matter all that much; but with more specific questions related to individual circumstances I think it definitely does. How many patients don’t ask pertinent questions because they don’t want the world to hear? Hopefully their corporate office will install something more private in the future.
Just where are pharmacists supposed to find the time to counsel patients? Most are already over-worked and over-tired. Case in point: I called my pharmacy 1 day ahead for 3 medication refills last week. The following day I arrived and my meds had not been filled yet (that happens more often than not). I waited, got my meds, checked the bottle label on each (just to check for any errors… Because you can’t be too careful), then I returned home and proceeded to fill my am/pm pill box when I noticed that one of the meds didn’t have the appearance of previous tablets. Turns out that I was given Xanax in error! The correct medication doesn’t resemble in any way the tablet shape or color of Xanax! 3 experienced pharmacists, no one in line behind me, and a mistake that could have ended badly had I not caught their error. And you want them to make time to counsel patients?? Not realistic!!
Lupie, This is a great response and a great question! Here’s what should happen… Pharmacists as a profession have been lobbying Congress for years to be granted “provider status” which essentially would allow them to bill for a patient visit, much like a nurse practitioner, although the pharmcotherapeutics training for pharmacists involves much more complex and advanced pharmaceutical science education. If this occurred, pharmacists could actually be employed by large medical practices to see patients that have multiple medications and complex issues around that. When pharmacies figured out a way to bill for vaccinations, corporate owners of large pharmacy supported it. What needs to happen is that pharmacists should be granted provider status and have a separate room for counseling within the pharmacy – some have already done this. Pharmacies could even employ a nurse practitioner to work in collaboration so that you have an urgent care of sorts that could perhaps reduce the overflow in ERs. There’s no question that pharmacists are trained for this – the questions are, do they have time when evaluated on how many RXs they can fill per hour, and will they be paid? See Nobody Knows. #RebrandPharmcy
Hi Mary,
The approach to Pharmacy that you discuss in your reply is EXACTLY how the VA pharmacy works. We first take a number, there are 3-4 private rooms with doors (numbers flash above each door, they call it the box). Once your number is up, you go into the little room, with a pharmacist behind a desk with a computer and a phone. They take your number, last name and last 4.
There is a chair for you also and they do ask all of the questions stated in the article. Only then is your Rx approved for filling, even refills.
Then you sit again in the waiting area and watch a large TV with many names, until your name pops up. Then you go to a separate set of windows, state your name and last 4, and the tech goes back and gets your meds for you.
It does take a while but all bases are covered and privacy is maintained.
JennS,
I’m glad to hear the VA is counseling patients in seperate private rooms and their system seems to be working. I can’t even begin to imagine how many patients they see in a day. I’m sure it can be very time consuming, painful, and frustrating from the patient side of things when there’s a long wait, but it’s good to know that they’re making an effort.
These are great “counseling” questions and needed but as RN I also recognize the significant amount of time this would take. A retail pharmacist would not have the time. Of course we should take the time but we know that a healthcare worker’s time is short and clients (patients) do not give direct answers. This would require an extra staff member at each level. At the hospital level it still takes an ungodly amount of time to just get the admission medications a patient is taking, and just as much time to reconcile on discharge. I guess my point is TIME. Seems as if so many different people are trying to help the physician do his job. All these questions need action and follow up from the physician who does not have the time or doesn’t take the time to counsel. Working for a physician I spent vast amounts of time educating patients and assisting in adjusting and readjusting and it was exhausting. I see that part of the problem as not having a clear plan in the beginning when treating pain initially.
Great post Dr. Fudin! Bu the flight attendant police are going to come get you! They’re not “stews” any longer – not in like 20 years! Wear the bow-tie, you might take pity and not tar and feather you!
Lynn McP
LOL Dr. McPherson. You never fail to make me smile.
Excellent point Dr. Fudin
Simple question.
How can a pharmacist decline a prescription when or if the said pharmacist is routinely facilitating a declination of prescription counseling?
Doesn’t this pendulum swing in two directions?
Terri, The laws differ by state. Some states require counseling on every new prescription. That can be interpreted two different ways. If the patient has been getting the exact same medication and dose of opioid, some states allow decline counseling. Since CII’s are not refillable, some states do require counseling because it’s not refillable and therefore is a new RX every month. But CIII and CIV are refillable and therefore counseling can be declined – these include Ultram (tramadol), Talwin (pentazocine), and Butrans/ Belbuca (buprenorphine). Soma (carisoproldol) is CIV and and so are benzidiazepines. Codeine in combo with acetaminophen, aspirin, or ibuprofen is a CIII and therefore refillable.
Excellent disctinction, thank you.