After viewing WKYC’s news report, Middletown official pitches ‘three strikes, you’re out’ Narcan plan, I was mortified to say the least. Middletown City Council member Dan Picard should be escorted out of his position promptly for even considering such a proposal and the citizens of the Cincinnati/Dayton metro area should be paving the road out.
Since when have people’s lives become a game? Perhaps some of the tax revenue from the Cincinnati Reds could help fund rehab for persons that have the disease of addiction, since according to Picard, human life is hinged on baseball game.
My goodness, Picard this gives the City of Flying Pigs a whole new meaning!
As you might have noticed, I think I was a bit too worked up to write this blog myself while maintaining civility. I therefore engaged our newest Pharmacy Pain Specialist, Dr. Erica Wegrzyn to mentor our new resident, Dr. Mena Raouf through a blog post to address this travesty. Neither of these professionals are new to this blogging on paindr.com, and once agian, they both did a fabulous job. In fact, on this one, THEY KNOCKED IT OUT OF THE PARK! Here is what they had to say.
Dr. Mena Raouf
In the midst of the opioid epidemic and rise in overdose related deaths, Middletown, Ohio is proposing a 3-strike policy on responding to overdoses.1
After the first two overdose rescues, the person would be required to perform community service for the equivalent amount of money used on the lifesaving response. After the third strike, the person is out of luck and the EMS service “wouldn’t dispatch” according to Middletown city council member, Dan Picard. “Last year, the department spent more than $11,000 on Narcan. This year, $30,000 has been spent on it.” Picard stated, “We’ve got to do what we’ve got to do to maintain our financial security and this is just costing us too much money”.1
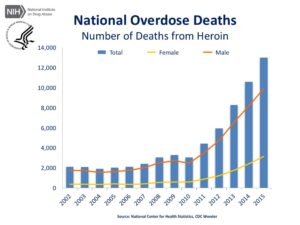
The rate of overdose deaths has been following a steady increase since 1999; however, there was a steep increase in the past few years despite recent policies to restrict opioid prescribing.2,3
Is this a coincidence? Did restrictions on opioid prescribing create another problem? While fatal overdoses involving semi-synthetic opioids (ex: oxycodone, hydrocodone, hydromorphone) fell between 2010 and 2015, the percentage of fatal overdoses involving heroin tripled.2 Ohio, in particular, had a 50% increase in heroin overdose deaths from 2011 to 2012 following opioid prescribing crackdown in 2011. The result is an increase in overall fatal overdoses involving opioids. 4
CLICK HERE IMAGE FOR LARGER VERSION
In Middletown, OH the number of overdoses increased from 532 in 2016 to 577 so far in 2017, an increase from 44 overdoses per month to 82 overdoses per month.1 What changed from 2016 to 2017? How come there is a sharp increase despite ‘policies to curb opioid use’? The CDC guidelines happened, encouraging prescribers to blankly implement the CDC recommendations on morphine equivalent dosing (MED), abruptly lowering patients to an MED of 50mg or 90mg.5 One plausible explanation for the stark rise in overdose deaths is that a subset of chronic pain patients on opioids who had their prescribed opioids abruptly discontinued turned to heroin use to help with withdrawal symptoms or to treat their chronic pain.
The point here is not on MED or CDC guidelines; these have been discussed in previous blogs. The point here is that among the Ohio overdoses , there are likely chronic pain patients who turned to heroin use to mitigate withdrawal symptoms after being cut off their opioids. This does not mean that substance abuse patients should be denied treatment. In fact, none should EVER be denied treatment based on comorbidities.
Denying patient treatment due to nonadherence is unethical and violates any code of healthcare profession ethics, let alone if the treatment is lifesaving. Are patients with other comorbidities who are nonadherent denied treatment? No. For example, in a different scenario, more than 25% of patients hospitalized for heart failure are readmitted within 30 days, with nonadherence (diet or medications) being the most common cause.6 In 2011, heart failure readmission cost $41.3 billion.6 Medication nonadherence costs $290 billion of avoidable healthcare costs.7 Are patients readmitted due to nonadherence denied treatment or subjected to community service to cover the treatment cost? No. Imposing community service requirements on non-adherent patients receiving lifesaving treatment because they have a comorbid psychiatric condition is stigmatizing and profiling.
Substance use disorders are often stigmatized more than other health conditions and viewed as moral and criminal issues, rather than a health concern.8-9 Unfortunately, the stigma discourages patients to seek help. The opioid epidemic is often sensationalized by media and exploited by policy makers looking for a quick fix and voter perception of “Hey, I solved the opioid epidemic”. Unfortunately, it is easily forgotten that no one chooses to develop substance use disorder, rather it is a medical condition that requires chronic management. 8-9
Treatment of opioid-use disorder requires a patient-centered approach. The strike clause imposed by Middletown on patients to do community service to cover the expense of naloxone is penny-centered. Instead, the focus should be efforts to provide help to patients with opioid use disorder and expand access to buprenorphine.
Dr. Erica Wegrzyn’s Perspective
With a long line of firefighters and emergency responders in my family, I became a volunteer firefighter in an effort to give back to my community. My position as an active interior firefighter often presents new and unique challenges, but in reality, the goal of every call is the same: preservation of life and property. This is a shared objective among fire service organizations including The Ohio State Firefighter’s Association (OSFA) whose bylaws indicate the following10:
The purpose and objectives of the OSFA shall be:
1. To promote and encourage the development of skills, knowledge and methods to prevent and combat injury, loss of life and property by fire, medical emergency or disaster.
2. To promote fellowship, good will, self-preservation and security among members of the OSFA and others engaged in similar services.
3. To encourage and support legislation which will prevent or reduce the loss of life or property of any individual or groups of individuals.
4. To accumulate and disseminate information for the purpose of encouraging and increasing membership in the OSFA and support of fire and emergency services.
Councilman Picard’s proposal to deny lifesaving services to a person suspected of an opioid overdose is in direct opposition of the mission of the fire service. As all first responders know, the details provided in the initial dispatch of a call often differ substantially from the actual scene upon arrival due to limited information often provided by laypersons on scene. Mr. Picard’s proposal to cancel emergency response is negligent, unproductive, and deadly. What if a family member of a substance abuser requires emergency medical attention? It is conceivable that the patient identity at initial dispatch could be unclear. What if a former substance user successfully achieves sobriety only to have a heart attack from coronary artery disease but dispatch cancels units in route due to his history. Is this justifiable? Speaking of heart attacks, cardiac arrest is the number one cause of firefighter line of duty deaths (LODD). Would it be ethical to cancel first response because a city councilman felt the firefighter consumed too much unhealthy food and beer? The point is, if a policy such as Mr. Picard’s three strikes proposal were to be permitted, then what is to say someone can’t arbitrarily select other disease states that “don’t warrant saving”.
Rather than condoning second degree murder for those with a psychiatric disease, the city of Middletown should look at ways to address this crisis at the source, such as education and outreach, rather than a “quick fix”.
My job as a clinical pharmacist is a parallel to that of my fire service, where my mission is to provide unbiased healthcare with the first and foremost goal to “do no harm”. Perhaps it is time we require our politicians to take the same oath.

So when is it acceptable to passively allow opioid overdose victims to die?
WHEN SECOND DEGREE MURDER IS LEGAL
AND , of course…
WHEN PIGS FLY!
As always, comments are welcomed!

Dr Mena Raouf, Pharm.D., is currently completing PGY-2 Pain and Palliative Care residency at the Stratton VA Medical Center in Albany, NY. Dr. Raouf received his PharmD from Albany College of Pharmacy and Health Sciences and completed a PGY-1 residency at the VA Tennessee Valley Healthcare System in Nashville, TN.

Erica Wegrzyn, B.S., Pharm.D. is the Clinical Pharmacy Specialist in Pain Management at the Stratton VA Medical Center, Albany NY. Dr. Wegrzyn received her Doctor of Pharmacy degree from Western New England university and went on to complete a PGY-1 general practice residency and recently completed a PGY-2 in Pain and Palliative Care. In addition to her work at the VA, Dr. Wegrzyn volunteers as a NYS class-A interior firefighter for Selkirk Fire District.
References
- http://news10.com/2017/06/27/ohio-city-considers-three-strike-policy-on-responding-to-overdoses/
- Centers for Disease Control and Prevention. Increases in Drug and Opioid Overdose Deaths — United States, 2000–2014. [Webpage on the internet]. January 1, 2016. Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6450a3.htm. Accessed June 28, 2017
- Atkinson TJ, Schatman ME, Fudin J. The damage done by the war on opioids: the pendulum has swung too far. Journal of Pain Research. 2014;7:265-268. doi:10.2147/JPR.S65581.
- Blackwell B. The heroin epidemic: death toll from drug continues to soar in Cuyahoga County. Cleveland state website. Available at: http://www.cleveland.com/metro/index.ssf/2013/09/heroin_epidemic_cuyahoga_count.html. Accessed June 28, 2017.
- Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49
- Gheorghiade M, Vaduganathan M, Fonarow GC, et al. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol. 2013 Jan 29;61(4):391-403.
- Iuga AO, McGuire MJ. Adherence and health care costs. Risk Management and Healthcare Policy. 2014;7:35-44. doi:10.2147/RMHP.S19801.
- Olsen and J. M. Sharfstein, “Confronting the Stigma of Opioid Use Disorder—and Its Treatment,” Jama, vol. 311, p. 1393, 2014. 2.
- “Substance Use Disorder Stop the Stigma and Expand Access to Comprehensive Treatment,” American Medical Association. [Webpage on the internet]. Available from: http://www.ama-assn.org/ama/pub/advocacy/topics/preventing-opioid-abuse/stigma-of-substance-use-disorder. Accessed June 28, 2017.
- Code of Regulations. The Ohio State Firefighter’s Association. 17 August 2014. Accessed 4 July 2017. Available: http://www.ohiofirefighters.org/Proposed%20Code%20Chnge%202017.pdf


Excellent post. Until deplorable politicians are voted out of office, I think we’ll see more horrific and painful policies like this. Frankly, you really have to wonder at the massive amounts of heroin that is entering our country and the relationships between organized crime and those who should be keeping our borders safe from heroin importation. But let’s instead worry about keeping brown people out.
On point! Well said!
Excellent and thoughtful blog. ER docs and other clinicians always seemed to get angry at patients that kept coming back messed up after the docs had tuned them up too in my experience. The adrenaline flows when first responders and clinicians are asked to help people in these high stakes and dangerous circumstances and thus there is a kind of countertransference to self destructive people that seems to always invite clinicians and others to pile on – even if it means ignoring the fact that you know the person has a chronic relapsing disease and you are in essence punishing them for their disease. I think a lot of policy makers mistakenly think that addicts are enjoying themselves and thus when we save them they think we are enabling them to further have fun at society’s expense. If only they really knew how bad an addict’s self inflicted suffering feels. I don’t know a good answer to all this (other than self reflection on our countertransfence) but it ain’t condemning people to death.
There is a dearth of social science education in healthcare professional curricula. Education of clinicians about pain management, opioids, and addiction should be holistic in approach during school. Also, leadership determines culture. Public display of compassionate patient care helps normalize appropriate behaviors.
Please comment on whether this attitude represents the “Darwinian approach” to opioid use disorders, and our system is avoiding discussing the “real” transparency attitudes of governmental or state regulatory policies on this issue.
More classic work, with Dr.s Raouf & Wegrzyn weighing in brilliantly! Outstanding job training Pharm.D.s who are not only technically brilliant, but principled as well!