Several opioid prescribing guidelines suggest or require that urine drug testing be the standard of care when prescribing chronic opioid therapy. Interestingly, these guidelines generally focus on chronic noncancer pain, and seldom if ever address alternatives in anuric dialysis patients as seen in Dialysis, Opioids, and Pain Management: Where’s the Evidence?. The latter two issues are subjects for subsequent blogs, but suffice it to say that I’ve seen my share of significant opioid diversion in both these populations.
Perhaps a more pressing question is why none of the current guidelines mention urine or blood analysis for monitoring chronic alcohol use, since opioid deaths are significantly more prevalent with concomitant use of alcohol and/or non-alcohol sedative hypnotics.
Here to help address this issue are budding young student pharmacists Mena Raouf and Lisa Dragic, aka #MenaLisa, a dual powerhouse that no doubt will eventually burgeon as pharmacist pain clinician leaders.
Here’s what #MenaLisa had to say…
Alcohol is sometimes sought by patients suffering from pain as a method of chemical coping in the presence of pain and associated psychiatric comorbidities including but not limited to anxiety and depression. Pain management in patients that consume alcohol can become complicated and puts the patient and opioid prescriber at-risk for complications and liability.
Taking a Look at The Facts
Alcoholism is the leading cause of morbidity and mortality in the United States and the prevalence has remained stable with 6% in men and 2% in women.1 It is estimated that the annual cost of US health care expenses related to alcohol (ethanol) consumption is $185 billion.1 More Americans die annually from alcohol than from illicit drugs of abuse. Ethanol is the leading cause of mortality in people 15 to 45 years of age.1 According to the Substance Abuse and Mental Health Services Administration’s Drug Abuse Warning Network (DAWN) there were 438,718 emergency department (ED) visits related to opioid pain relievers. Of the opioid pain reliever ED visits, an estimated 81,365 (18.5%) involved alcohol. It was reported that 3,883 deaths were linked to opioid pain relievers and of that, 860 (22.1%) involved alcohol.2 While we don’t know how many of the subjects were actually prescribed opioids v. using them illegally, testing for alcohol use when prescribing opioids has heretofore been generally disregarded short of simply questioning the patient. Surely alcohol screening is not a part of the standard urine testing by immunassay panel.
Addiction 101
Addiction is a complex disease that affects the brain by altering its chemistry. Drugs cause disruption to the brain by imitating the brain’s natural chemical messengers and some drugs even have similar structures to natural chemical messengers in the brain that cause central nervous system release of various neurotransmitters such as dopamine. There is no one factor that makes a person addicted to drugs or alcohol. Some anti-opioid zealots have suggested that opioids alone are the gateway to a spiraling addiction disorder in the majority of patients. But, that begs the question of why the world majority are not comprised of alcoholics. This has been discussed may times by renowned psychologist Dr. Steve Passik; “First, you have to have a drug with rewarding properties. Second, you have to give that drug to a vulnerable person. Third, that person must use that drug at a vulnerable time. In pain management, we have exposure to drugs with rewarding properties and all of our patients are going through a vulnerable time.”
We do know that people are born with certain genes, and these genes may predispose them to addiction. Thus, if you have a rewarding drug (or alcohol) in a vulnerable person at a vulnerable time with this predisposition, it may create the perfect storm for a downward spiral to addiction. Again, while some may argue that addiction is a choice, if genetic makeup weren’t a factor than everyone would be addicted to alcohol and opioids. But, for many, this isn’t the case- some may have an occasional drink and are just fine – same for opioids.
Why Should we monitor alcohol use?
Alcohol comes with drug interactions and could increase exposure and/or potentiate effects of commonly used analgesics. There are pharmacokinetic and pharmacodynamic interactions associated with concomitant alcohol-opioid use.2 One of the most concerning interactions is alcohol-induced dose dumping; dose dumping is defined as “unintended, rapid drug release in a short period of time of the entire amount or a significant fraction of the drug contained in a modified release dosage form”. 4 For instance, concomitant administration of alcohol with Palladone (extended-release hydrocodomorphone, withdrawn from the US market for this reason) resulted in up to 16-fold higher plasma concentrations of hydromorphone.5 In vitro FDA studies revealed that when Avinza (extended release morphine) was mixed with ethanol, there was a more rapid release of morphine.4 The additive central nervous system and respiratory depressant effects from the high opioid peaks coupled with alcohol, which could lead to fatal poisoning.7
But I use non-opioid analgesics, so does it still matter?
The answer is yes! There are safety concerns with concomitant alcohol use and other commonly used analgesics. Combined alcohol use with non-steroidal anti-inflammatory drugs (NSAIDs) could increase bleeding risk and cause eshophageal hemorrhage.8 Alcohol depletes glutathione and could predispose persons to hepatotoxicity with acetaminophen use.9,10 Alcohol could increase the sedative effects of antidepressants (amitriptyline, mirtazapine), skeletal muscle relaxants (cyclobenzaprine, carisopridol) and anticonvulsants (benzodiazepines, gabapentinoids, barbiturates) all of which are commonly used for chronic pain syndromes.9 The concurrent administration of all centrally acting drugs such as opioids and those listed above combined with alcohol can increase the risk of sedation, drowsiness , overall mental impairment, and opioid-induced respiratory depression.
But again, alcohol monitoring is largely ignored as a standard monitoring parameter when prescribing opioids.
There is a need for evaluating and monitoring alcohol consumption when managing various pain conditions. Fortunate for patients and providers, various screening tools and biomarkers may be used to monitor alcohol consumption.
Risk Assessment Tools12
There are screening questionnaires that could used to evaluate alcohol use in patients
- NIDA Drug Use Screening Tool: Quick Screen
- Alcohol Use Disorders Identification Test (AUDIT)
- CAGE
- CAGE-AID
- CRAFFT
And of course, there are biomarkers that could be used to identify alcohol consumption and monitor for sobriety.
But First…. Let’s take a look at how the body handles this cocktail
Ethanol Pharmacokinetics:
Following alcohol intake, 80% is rapidly absorbed in the intestine and 20% is absorbed in the stomach.13,14 There are certain factors that can boost or slow down the absorption of ethanol. Some factors that may enhance the absorption include ethanol intake without food, dilution of ethanol, and carbonation. Factors that may decrease absorption include presence of food, co-ingestion of xenobiotics such as aspirin and N-butylscopolamine. Once absorbed, it is distributed into the total body water.14,15
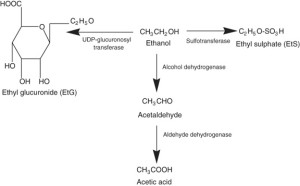
Approximately 90-95% of ethanol is oxidized in the liver by alcohol dehydrogenase and 2-5% is excreted unchanged by the kidneys, lungs, and sweat.13-15 Due to the rapid metabolism and ethanol and excretion the time frame for positive saliva, breath, or blood is limited to <12 hours. Thus, the oxidative products of ethanol must be measured in short period post ethanol consumption. Less than 0.1% undergoes phase II conjugation to produce ethyl glucuronide and ethyl sulfate. 13-15
Metabolism of Ethanol Following Ingestion15
Biomarkers for short-term use
Ethyl glucuronide (EtG) and Ethyl sulfate (EtS) are conjugated direct metabolites of recent ethanol consumption. EtG is formed by a reaction between ethanol and uridine-5-diphospho-β-glucuronic acid which is catalyzed by an enzyme called UDP-glucuronosyltransferase (UGT). 14 Ethyl sulfate (EtS) is formed by conjugation with a sulfate involving cytosolic sulfotransferase.13-15
Ethyl Glucuronide and Ethyl Sulfate15
These metabolites can be detected several days after ethanol has already been eliminated. Over the past years, the use of non-oxidative biomarkers to detect ethanol consumption has become of increasing interest because these metabolites provide strong indication of recent drinking. The standard for detecting alcohol use for many years has been blood-based biomarkers and often times they are suboptimal. As depicted immediately above, EtG and EtS can be detected for up to 5 days after ethanol has been eliminated from the body.14 These metabolites are detectable in urine for ≤24 h after intake of ≤0.25 g/kg ethanol, and for ≤48 h after intake of ≤0.50 g/kg ethanol.5 While these biomarkers have many advantages over traditional ways of measuring ethanol, it should be noted EtG can be produced post-sampling if specimens are infected with E. Coli and contain ethanol.17 Therefore, the use of EtS could be advantageous in patients with suspected urinary tract infections.
| Marker | Half-life | Time to return to normal limits | Type of drinking characterized | Comments |
| Ethyl glucuronide | 2-3 hours | 3–4 days | Identifies low–level consumption | Can be measured in urine or hair |
| Ethyl Sulfate | 2-3 hours | 3–4 days | Identifies low–level consumption | Can be measured in urine or hair |
Biomarker for chronic use
Gamma-Glutamyltransferase (GGT) is a glycoenzyme that transfers gamma-glutamyl functional group of glutathione to accepting molecule.18 GGT becomes elevated with accelerated synthesis or release from damaged hepatocytes. GGT is the most widely used biomarker for alcohol abuse and measured to assess abstinence. It used to assess chronic rather than episodic drinking.18,19 Levels typically rise with chronic heavy alcohol intake and returns to normal limits with 2-6 weeks of abstinence.18 It is important to note that GGT could be elevated with hepatobiliary disorders, smoking, cardiovascular disease, and with certain medications including phenytoin, carbamazepine, and barbiturates. 20,21,22
Other Markers for Heavy Drinking 12
| Marker | Time to return to normal limits | Type of drinking characterized | Comments |
| Gamma–glutamyltransferase | 2–6 weeks of abstinence | ∼ 70 drinks/week for several weeks | Many sources of false positives |
| Aspartate aminotransferase | 7 days, but considerable variability in declines with abstinence | Unknown, but heavy | Many sources of false positives |
| Alanine aminotransferase | Unknown | Unknown, but heavy | Many sources of false positives
Less sensitive than aspartate aminotransferase |
| Macrocytic volume | Unknown but half–life ∼ 40 days | Unknown, but heavy | Slow return to normal limits even with abstinence |
| Carbohydrate–deficient transferrin | 2–4 weeks of abstinence | 60+ g/d for at least 2 weeks | Rare false positives
Good indicator of relapse |
It remains a dilemma in pain management where patients with true pathologies and legitimate pain seek alcohol for chemical coping. The presence of concurrent alcohol abuse disorder does not negate the legitimacy of the patient’s pain complaints, but it may pose safety concerns with the use of pharmacologic analgesics as highlighted above. The patient must be willing to work with the healthcare team to receive treatment for both disorders; that is a choice the patient has to make.
Urine Drug Testing
Urine Drug testing has become an important component when treating pain patients with chronic opioid therapy. It is not enough to rely on self-reporting of substance use.23 Urine Drug Testing has become the standard of care because it can help monitor compliance, screen for new or recurrent drug misuse, and assist in diagnosis of patients. Urine Drug Testing is still underutilized.23,24 In fact, one audit of medical records found that only 8% of primary care providers utilized UDT.25 According to the DAWN study, 22.1% of opioid deaths involved alcohol.2 This begs the question of why biomarkers such as ethyl glucuronide (EtG) not included in the standard of care since such an alarming number of opioid deaths are in fact related to alcohol consumption. Discussions of concomitant alcohol as a significant contributor to opioid-related deaths has been largely ignored by the sensationalistic media frenzy. Little is written in mainstream media to suggest that patients should bear a significant part of the responsibility if they choose to drink while consuming alcohol. It note that that prescribers and pharmacists should diligently warn against alcohol combined with any of the drugs listed above and that patients should seriously heed the auxiliary label warning on the bottle along with handout material supplied with their medications.
In summary, perhaps we need a paradigm shift that considers ethyl glucuronide as part of the standard urine screen. This could enhance patient safety and altert prescribing clinicians that their patient needs substance abuse counseling with focus on alcoholism to ensure mediation safety and minimize risks.
As always, comments are welcome!
This article was collaboratively written with Lisa Dragic and Mena Raouf whose bios appear below.

Lisa Dragic is a 2016 Doctor of Pharmacy candidate at Temple University School of Pharmacy. Lisa is completing her last professional year as a student pharmacist with an interest in pain management, addiction, infectious disease, and palliative care. She hopes to complete a PGY-1 and PGY-2 pharmacy residency. Lisa aspires to be a leader in her chosen profession with focus on patient advocacy.
Mena Raouf, a 2016 PharmD Candidate at the Albany College of Pharmacy and Health Sciences completing his last professional year as a student pharmacist, with a concentration in Nephrology. Mena moved from Egypt 5 years ago to start pharmacy school and career in the U.S. He hopes to complete PGY1 and PGY2 Pharmacy Residency and practice as a clinical pharmacist specialist. He is currently under the mentorship of Dr. Jeffrey Fudin studying pain management.
References
- Yip L. Ethanol. In: Hoffman RS, Howland M, Lewin NA, Nelson LS, Goldfrank LR. eds. Goldfrank’s Toxicologic Emergencies, 10e. New York, NY: McGraw-Hill; 2015. http://accesspharmacy.mhmedical.com.libproxy.temple.edu/content.aspx?bookid=1163&Sectionid=65098321. Accessed February 5, 2016.
- gov. Alcohol Involvement in Opioid Pain Reliever and Benzodiazepine Drug Abuse–Related Emergency Department Visits and Drug-Related Deaths — United States, 2010. 2016. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6340a1.htm#Tab1. Accessed February 15, 2016.
- gov. Understanding Drug Abuse and Addiction. 2016. Available at: https://www.drugabuse.gov/publications/drugfacts/understanding-drug-abuse-addiction. Accessed February 15, 2016.
- http://www.fda.gov/ohrms/dockets/ac/05/briefing/2005-4187B1_01_08-Alcohol-Induced.pdf
- http://www.fda.gov/CDER/Drug/InfoSheets/HCP/hydromorphoneHCP.pdf
- http://www.fda.gov/MEDwatch/safety/2005/avinza_PI.pdf
- Gudin J, Mogali S, Jones J et al. Risks, Management, and Monitoring of Combination Opioid, Benzodiazepines, and/or Alcohol Use. Postgrad Med. 2013 Jul; 125(4): 115–130.
- Sutton R1, Shields R. Alcohol and oesophageal varices. Alcohol Alcohol. 1995 Sep;30(5):581-9.
- Licht H, Seeff LB, Zimmerman HJ. Apparent potentiation of acetaminophen hepatotoxicity by alcohol. Ann Intern Med 1980; 92: 511-6.
- Black M, Cornell JF, Rabin L, Shachter N. Late presentation of acetaminophen hepatotoxicity. Dig Dis Sci 1982; 27: 370-4
- Weathermon R, Crabb DW. Alcohol and Medication Interactions. Alcohol Research & Health 1999; 23;1: 40-53
- National Institute on Alcohol Abuse and Alcoholism. Biomarkers of Heavy Drinking. August 2004. Available from: http://pubs.niaaa.nih.gov/publications/AssessingAlcohol/biomarkers.htm Accessed February 8 2016
- Holford NH. Clinical pharmacokinetics of ethanol. Clin Pharmacokinet. 1987 Nov;13(5):273-92.
- Jones A.W.. Urine as a biological specimen for forensic for forensic analysis of alcohol and variability in the urine-to-blood relationship. Toxicol Rev. 2006; 25(1):15-35.
- com. Warde Medical Laboratory. 2016. Available at: http://www.wardelab.com/19-3.html#F2. Accessed February 5, 2016.



Hello, I just started going to pain management, they took a urine sample 1st visit, then I went in the next month for cortisone shots in my neck. The nurse said, we found alcohol in your test, but no opiates! I said I didn’t have any before going there, she said, well, this better not happen again? I sometimes have a couple drinks, on occasion, I don’t really understand.
Alcohol detection is from several days ago. It’s not alcohol – it’s the metabolite. See Should alcohol monitoring be a standard of care when prescribing opioids?
I manage a Pain Management clinic and we do LC-MS testing for Alcohol, among other things. We struggle with where to draw the line when a patient consistently is testing positive for alcohol and continuation of opioid therapy. We always warn patients on the possible negative side effects, have an alcohol risk assessment done, and have even weaned patients who have consistently tested positive. From your perspective, should there be a line in the sand? Should patients with higher MED not be allowed to continue opioid therapy if testing positive for alcohol? Should you not allow it all because of the liability? What are your thoughts?
Brenna,
We monitor EtG levels. If a patient is actively drinking, we will not prescribe opioids because of the inherent risk. In fact, we generally will not prescribe any meds but will offer alternatives. This is because any of the APAP/opioid combos are problematic due to liver toxicity and OIRD respectively as you know, increased risk of GI bleed from NSAID or SNRIs with alcohol, and increased sedation and/or falls with anticonvulsants. Our feeling is that if a patient’s pain is bad enough they have to choose between alcohol and drugs. Since I have no control over the former in terms of amount or frequency, from a liability and safety perspective, i feel I have limited options.
Great article, Jeff.
Our system’s drug and alcohol center uses phosphatidylethanol. Window of detectability goes much further back. I’ve used it for complete abstinence monitoring in my alcoholics prescribed opioids.
https://www.dnalegal.com/sites/default/files/uploads/files/PEth%20Testing%20-%20Brochure.pdf
Thank you for this informative article! In New Mexico 51% of overdose deaths in 2014 involved alcohol. In my own community alcohol causes more deaths than any other drug, yet as soon as opioids show up then any discussion of other drugs ceases. I just watched the Frontline episode on the heroin epidemic (I dislike the use of this word in this context) and one of the young people started off on alcohol and marijuana and then tried cocaine and then wound up on heroin. This was a truly vulnerable young person but her death is counted as one more heroin overdose and lost in the narrative was the complexity of understanding the pathway to addiction. And the voice of the chronic pain patient fades into the background!
Thank you for your informative article. I do regularly test for alcohol for UDT.
Can one detect ethanol or metabolites from consumption of viscous xylocaine (0.1% alcohol), or even exposure to mouthwashes?
i have heard of clients who frequently wash with hand sanitizers can have small exposure for alcohol metabolite detection.
Diabetics may have glucose fermentation in their urine.
Please clarify any other legitimate sources of alcohol or its metabolites that might occur in patient monitoring for consideration.
Howard, Thanks for the comment. The amount of alcohol and absorption in topical products is too low to affect ethyl glucuronide in any meaningful way, and if it was high enough, it is too volatile to be absorbed anyway, as it will dissipate prior to absorption. Aside from that, the 0.1% found in viscous xylocaine is so so small, it will not contribute. Anybody that tells you this has probably prepared an excuse in advance.
Interesting blog, and the issue of alcohol use and abuse is indeed virtually absent in the media and medical-regulator frenzy to restrict the legitimate use of opioids. Before I retired I was providing chronic opioid and other non-interventional management to several hundred chronic pain sufferers. In the latter part of my years in practice, UDTs became routine, and almost all patients receiving opioids underwent monthly UDT. In all of those tests, only 2 came back as positive for ethanol. Neither of those patients showed persistence of ethanol, and one was deemed NOT to be suffering from alcohol abuse after an evaluation by a local drug treatment program. The average duration of pain among my patients was 15 years when I did retire, and I had a very stable patient population.
I raise this issue because the prevalence of alcohol use in my group of truly chronic pain patients was quite low. That is in stark contrast to the 22% of people dying from opioid overdose having alcohol in their system. Perhaps this is another piece of evidence that stable chronic pain patients are NOT the population that is committing suicide.
One other note, a group of researchers in Philadelphia analyzed alcohol purchasing patterns in poor neighborhoods and those with more disposable income. They found that there was significantly less per capita alcohol consumption among the low income population. (I apologize for not having a reference, but I heard it at one of the conferences for the American Public Health Association that was held in Philadelphia.) It is also true that many, probably the majority, of my patients were on Social Security Disability or SSDI, and had barely enough income to survive.
It is rare to see any statistics about socioeconomic data about chronic pain patients and the other group of people who are dying from overdose. Alcohol use or non-use may be a useful marker to distinguish at least some of the people making up these two disparate albeit overlapping groups of people.
It is a great service for the authors of this blog to raise this important issue.
Thank you for this excellent article! I definitely agree that alcohol should be tested. As a pain patient who does not drink alcohol, I believe that the CDC is now using the 16,000 deaths per year due to drug overdoses to give validity to preventing legitimate patients from getting pain meds in Florida without considering those deaths could have been due to alcohol consumption.
It blows my mind when I think how many HUNDREDS OF THOUSANDS of deaths will occur if pain patients are refused their pain meds. Why is the CDC involved, anyway?
So let the urine tests include alcohol! It may just save us from dying horrible deaths from untreated pain!